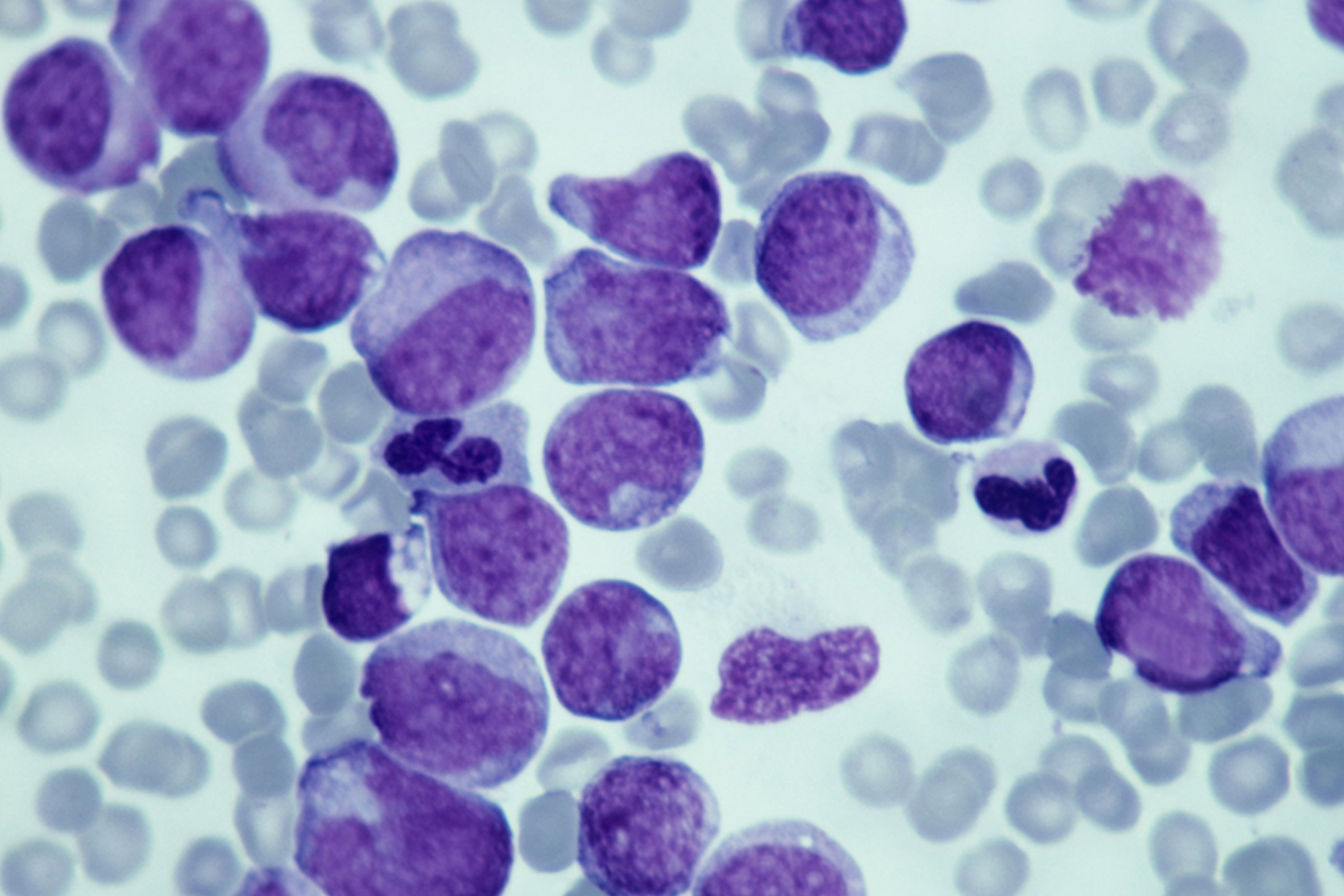
Childhood leukemias strike different types of blood cells and progress at different speeds. The main treatment we use for most blood cancers is an allogeneic bone marrow transplantation (BMT), which uses healthy stem cells from a donor. (Stem cells are undifferentiated cells with the ability to become specific cell types.) After high-dose chemotherapy and radiation therapy, the transplanted stem cells restore the patient's bone marrow, which is where most of the body’s blood cells are made.
At UCSF, we use BMT to treat acute lymphoblastic leukemia (ALL), acute myelogenous leukemia (AML) and chronic myelogenous leukemia (CML). BMT is also a therapy for the bone marrow disorders known as myelodysplastic syndromes (MDS), which can lower blood cell counts of certain blood cells. This is often called a pre-leukemia syndrome because patients with MDS have a significantly increased risk of developing leukemia.
Our BMT program offers transplantation from:
- Related donors, including siblings and parents, and in some cases, more distant relatives, such as cousins and grandparents
- Matched unrelated donors, including stem cells from umbilical cord blood
The advantage of using a donor's marrow cells – rather than the patient's own – is that it provides a "graft-versus-leukemia effect," in which the donor's healthy bone marrow cells kill residual leukemia cells, decreasing the chance of a relapse.
But transplanting cells from a donor does carry the risk of graft-versus-host disease, a complication in which the donor's cells attack healthy cells in the recipient's body. The condition can affect the skin, liver and many other organs, and requires treatment with immunosuppressive drugs.
Who is a candidate for a BMT?
There are four basic categories of patients for whom we consider BMT:
- High-risk leukemia patients in their first remission –
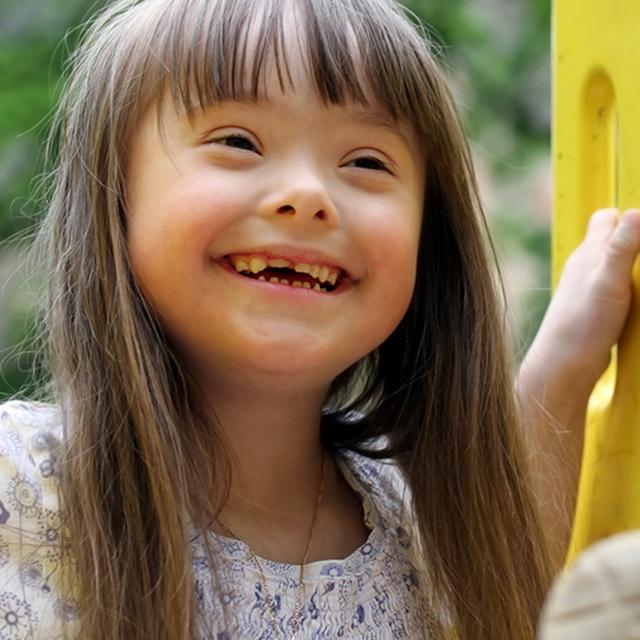
When a matched donor is available, our program provides transplantation for high-risk leukemia patients in their first remission. In very high-risk patients, such as children with leukemia who don't achieve a first remission with chemotherapy, an unrelated donor transplant can be performed as soon as remission is achieved. Eligible patients in this category include:
- Children with AML
- Children with high-risk ALL
- Infants with leukemia
- Certain children even if not in complete remission
- Patients with myelodysplastic syndromes – Children with MDS are eligible for transplant as soon as the diagnosis is established.
- Patients with acute leukemias whose disease has relapsed – We can perform a transplant in these cases once the leukemia is considered to be in remission, which is when no sign of the disease is seen in the bone marrow. Remission can be achieved using chemotherapy and total body irradiation. This is called the conditioning regimen and is performed prior to transplantation. Our program also offers research protocols investigating whether using additional donor T cells after the transplant may decrease the likelihood of recurrence.
- CML patients – When children with CML can't be put into complete remission with chemotherapy, they should receive a BMT from either a related or an unrelated donor as early as possible. Currently, we offer a protocol under investigation that utilizes an optimal dose of a potent chemotherapy drug called busulfan along with fludarabine, a drug that effectively prevents rejection of the donor cells with a reduced-intensity regimen.