Autoimmune Hepatitis

Overview
Unlike other forms of hepatitis, such as viral and toxic hepatitis, autoimmune hepatitis occurs when the body's immune system mistakenly attacks healthy liver cells. As a result, the liver becomes inflamed and hepatitis develops. In severe cases or if left untreated, the condition can lead to scarring of the liver, a condition known as cirrhosis, and ultimately to liver failure.
Research has shown that genetic factors may increase some people's risk of developing autoimmune hepatitis. While people of any age can develop autoimmune hepatitis, women between the ages of 20 to 40 are most commonly affected.
Our approach to autoimmune hepatitis
UCSF offers the most advanced diagnostic and treatment options for patients with autoimmune hepatitis. We generally begin with a high dose of prednisone (a steroidal medication) to stop or slow the immune system's attack on the liver. We then taper the dose and may supplement the regimen with additional immune-suppressing medications to manage the condition long term.
Autoimmune hepatitis can lead to severe liver damage or failure. In these cases, a liver transplant may be necessary. Our liver transplant program, designated a center of excellence by the U.S. Department of Health and Human Services, is known for outstanding outcomes and for helping pioneer techniques that have made transplants safer and more successful. We perform more than 100 transplants each year, and our survival statistics are among the best in the country.
Awards & recognition
-

Among the top hospitals in the nation
-

One of the nation's best in gastroenterology & GI surgery
Signs & symptoms
Symptoms of autoimmune hepatitis vary, depending on the severity. However, some of the more common include:
- Fatigue
- Enlarged liver
- Jaundice, a condition that causes a yellowing tint of the skin and eyes
- Joint pain
- Abdominal discomfort
- Blood vessels that appear as "spiders" on the surface of the skin
- Nausea
- Vomiting
- Loss of appetite
- Dark urine
- Mental confusion, which may occur in advanced stages
Diagnosis
In making a diagnosis of autoimmune hepatitis, your doctor will start by conducting a thorough physical examination and asking about your medical history, including any symptoms you have been experiencing.
You may also receive the following tests:
- Blood Tests. A series of blood tests will be conducted to detect any antibodies that indicate autoimmune hepatitis and liver injury. In addition, blood tests help to distinguish which type of hepatitis you have.
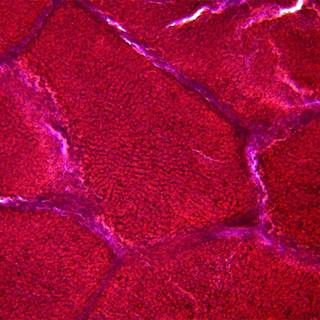
- Liver Biopsy. Because diseases other than autoimmune hepatitis can give rise to these antibodies, a liver biopsy often is done to establish the diagnosis. During a biopsy, a small sample of tissue is removed from your liver using a thin needle. The tissue is prepared and stained in a laboratory for examination under a microscope.
Treatments
A drug called prednisone is the cornerstone of treatment for autoimmune hepatitis. It is initially given in high doses, which are tapered when the liver begins to respond.
The optimal length of prednisone treatment is uncertain. Because many patients relapse after relatively brief treatment, most doctors recommend prednisone at the lowest effective dose for one to two years before stopping. The long-term outlook depends on the success of the patient's initial treatment.
For patients who are resistant to prednisone, other types of immunosuppression may be tried. Liver transplantation is the treatment for cases that progress to liver failure.
Liver transplantation
Liver transplant is recommended for people whose autoimmune hepatitis causes severe liver damage or progresses to liver failure. The evaluation for a transplant is complex and generally requires several months. Therefore, even if a patient is feeling well, they should be referred for a transplant at the first sign of liver failure or if they have advanced liver disease diagnosed by X-ray studies or liver biopsy.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.
More treatment info
-
Living Donor Liver Transplant
The liver's unique ability to regenerate itself enables life-saving transplants.
Learn more -

Liver Transplant
Liver transplantation can be a life-saving option for patients with end-stage liver disease. Learn what happens during the evaluation, surgery and recovery.
Learn more