Myeloproliferative Disorders
Overview
Myeloproliferative neoplasms, or MPNs — also called myeloproliferative disorders, or MPDs — are a collection of blood disorders that are believed to be caused by mutations in bone marrow stem cells. These stem cells normally give rise to mature cells found in the blood, such as red blood cells, which carry oxygen, white blood cells, which fight infection, and platelets, which facilitate blood clotting. In MPN, mutations cause the affected stem cells to produce an abnormal number of these cells. More than 200,000 people in the U.S. are estimated to be living with an MPN.
Generally, MPNs are associated with an overproduction of some of the mature blood cell types. Polycythemia vera is an MPN associated with too many red blood cells; essential thrombocythemia refers to the abnormal overproduction of platelets, and chronic myeloid leukemia is generally associated with too many white blood cells.
Many people with these conditions have few, if any, symptoms, but complications can occur, including stroke in patients with poorly controlled disease. MPNs can sometimes transform to leukemia or to myelofibrosis, an MPN that is characterized by excessive scar-type tissue in the bone marrow.
The molecular causes of the majority of MPN cases have been identified — mutations in the genes JAK2 and ABL are found in nearly all patients with polycythemia vera and chronic myeloid leukemia, respectively. This knowledge has led to the development of targeted therapies that shut off the activity of these overactive mutant proteins. In the case of chronic myeloid leukemia, the outlook of patients has been transformed dramatically as a result.
Our Approach to Myeloproliferative Disorders
UCSF is dedicated to delivering the most advanced treatments for myeloproliferative disorders with care and compassion. There are several types of myeloproliferative disorders, and the best therapy depends on the type and the patient's symptoms. In general, the goal of treatment is to bring the blood cells back to normal levels. Patients who aren't experiencing symptoms may not need immediate treatment but require careful monitoring.
We are also dedicated to discovering better treatments for myeloproliferative disorders through research. Interested patients may have the option to participate in clinical trials of potential new therapies.
Awards & recognition
-

Among the top hospitals in the nation
-

Best in Northern California and No. 7 in the nation for cancer care
-

blood and marrow transplants performed each year
Signs & symptoms
Patients with MPN may have many or few symptoms depending on how abnormal their blood counts become.
Those with essential thrombocythemia and polycythemia vera have "thick" blood that is more prone to clotting and is associated with heart attacks, strokes and clots in leg veins. Patients with chronic myelogenous leukemia and myelofibrosis often feel tired and report pain or fullness in their belly from an enlarged spleen.
Patients with MPN may have moderate or severe anemia, a condition where there are not enough red blood cells to carry oxygen. Other signs and symptoms may include:
- Shortness of breath during exertion
- Weakness and fatigue
- Pale skin
- Loss of appetite
- Prolonged bleeding from minor cuts due to low platelet counts
- Purpura, a condition in which the skin bleeds, causing black and blue or pin-sized spots on the skin
- Sinus, skin or urinary infections due to low white blood cell counts
Diagnosis
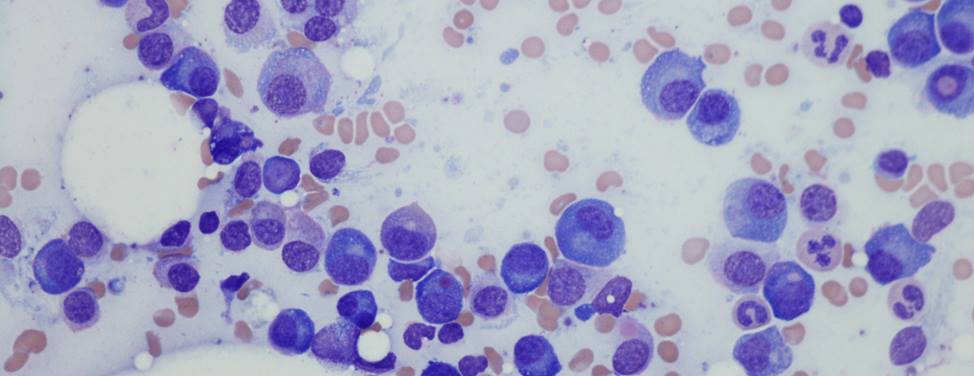
When an MPN is suspected, blood tests are conducted that count the number of different cells in the blood. If the results are abnormal, other blood tests may be ordered.
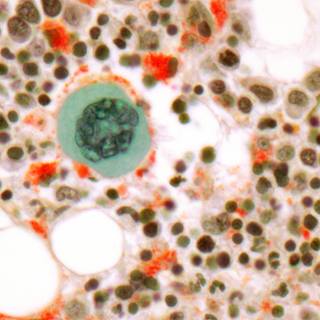
A bone marrow biopsy is performed to confirm a diagnosis of MPN. During this test, a needle is inserted into the bone and marrow is extracted. The sample is then carefully examined under a microscope by a pathologist.
Treatments
Although myeloproliferative neoplasms usually cannot be cured, there are treatments for all patients with the condition. Treatment of MPNs depends on the type and on the presence of symptoms. In general, treatment aims to correct the abnormal blood counts.
Some people don't experience any symptoms and therefore don't require treatment.
Low dose chemotherapy pills, such as hydrea, can be given to patients with essential thrombocythemia and polycythemia vera to lower their platelet and red blood cell counts. Phlebotomy (the removal of blood intravenously) is also an effective strategy for lowering red blood cell counts and controlling symptoms.
The treatment of choice for chronic myelogenous leukemia is a new anti-leukemia medication, called Gleevec. Testoterone therapy can sometimes improve anemia in patients with myelofibrosis. Other potential therapies for myelofibrosis include chemotherapy, radiation therapy, thalidomide and alpha interferon. In addition, patients with myelofibrosis frequently require red blood cell transfusions.
Chemotherapy
Chemotherapy uses drugs to kill extra blood cells in the body. Chemotherapy may be taken orally in a pill format or may be administered intravenously (through an IV). Chemotherapy is called a systemic treatment because the drug enters the bloodstream, travels through the body and can kill cells throughout the body.
Radiation Therapy
Radiation therapy uses high-energy X-rays to kill cells and is sometimes used to relieve symptoms of MPN. External beam radiation therapy, which uses a machine outside the body to administer the radiation, is usually the type of radiation therapy used to treat MPN. In addition, a radioactive drug called P32 can be given intravenously to lower the number of red blood cells made by the bone marrow.
Surgery
Surgery to remove the spleen, called a splenectomy, may be performed if a patient's spleen is swollen.
Biological Therapy
Biological therapy is being tested as a possible treatment of MPN. This type of therapy uses materials made either by the body or in a laboratory to boost, direct or restore the body's immune system. Biological therapy sometimes is called biological response modifier (BRM) therapy or immunotherapy.
Hormones
Hormones may be used in certain instances to treat side effects of MPN. In patients with agnogenic myeloid metaplasia, hormones called glucocorticoids may be given to increase the life span of red blood cells. In addition, hormones called androgens sometimes are used to stimulate the bone marrow to produce more blood cells.
A person's recovery or response to therapy depends on their type of MPN, age and general health. Most people with essential thrombocythemia and polycythemia vera live more than 10 to 15 years with few complications. People with myelofibrosis live approximately five years and in some cases, the disease may develop into acute leukemia.
Stem Cell Transplantation
The only curative therapy for MPN (excluding chronic myelogenous leukemia) is allogeneic stem cell transplantation, which is the transfer of stem cells from one person to another.
Whether stem cell transplantation is an appropriate therapy for an individual patient depends on a number of factors including age, MPN subtype, current symptoms or the extent of disease and the availability of a donor. We encourage patients to consult with a stem cell transplantation doctor to learn more about MPN, possible treatments and stem cell transplantation.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.
Recommended reading
Where to get care (1)
Related clinics (4)

Osher Center for Integrative Health
 2
2