Rectal Cancer
Overview
What is rectal cancer?
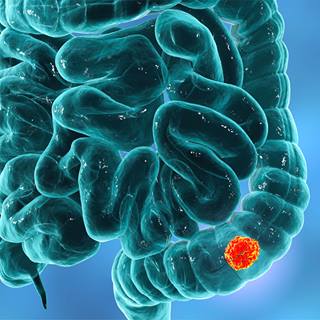
Rectal cancer occurs when cancerous cells develop in the tissue of the rectum. The rectum is the last part of the large intestine and leads to the anus, which is the opening to the outside of the body. Body waste is stored in the rectum until it is eliminated through the anus as a bowel movement.
Rectal cancer is closely related to colon cancer, and the two are often discussed together as colorectal cancer. Colorectal cancer ranks third in cancer-related deaths for both men and women in the United States.
Although rectal cancer is a life-threatening disease, it is highly curable if found early. Therefore, regular checkups and colorectal cancer screenings are important.
Our approach to rectal cancer
Specialists at UCSF have decades of experience with diagnosing and treating rectal cancer. We focus on providing the most effective care for each patient. Surgery is the most common treatment for all stages of rectal cancer, and we use the latest surgical approaches. Many patients will also have radiation, chemotherapy or both.
Our team treats people at every stage of rectal cancer and often handles complicated or unusual cases that other hospitals turn away. We also offer patients opportunities to receive promising new treatments by joining a clinical trial.
Awards & recognition
-

Among the top hospitals in the nation
-

Best in Northern California and No. 7 in the nation for cancer care
-

Designated comprehensive cancer center
Risk factors for colorectal cancer
Although the exact causes of rectal cancer are unknown, certain factors have been identified that may increase a person's chance of developing the disease. These same factors also increase the risk of colon cancer. They include:
- Age. Most rectal cancers are diagnosed in people age 50 or older, although the disease affects all ages.
- Bowel disease. A history of colorectal cancer, intestinal polyps or inflammatory bowel disease (ulcerative colitis or Crohn's disease).
- Diet and exercise. A diet high in fat, particularly from animal sources, and a sedentary lifestyle.
- Ethnic background and race. Jews of Eastern European descent (Ashkenazi Jews), African Americans, Native Americans and Alaska Natives have higher rates of colorectal cancer.
- Family history or genetic factors. Specific genes may significantly increase a person's chance of developing colorectal cancer. People with a strong family history – defined by cancer or polyps in a first-degree relative (parent, sibling or child) under 60 years old or two first-degree relatives of any age – are at elevated risk.
- Smoking and alcohol. Research suggests that smokers and heavy drinkers have an increased chance of developing rectal cancer.
Symptoms of rectal cancer
Common signs of rectal cancer include:
- A change in bowel habits
- Diarrhea, constipation or a feeling of incomplete emptying during bowel movements
- Blood in the stool, either bright red or very dark
- Stools that are narrower than usual
- Abdominal discomfort, such as frequent gas pains, bloating, fullness or cramps
- Weight loss for no known reason
- Always feeling tired
- Vomiting
Diagnosis of rectal cancer
To diagnose rectal cancer, doctors start by reviewing your medical history. They'll ask about any symptoms you're experiencing and then conduct a thorough physical exam. They also may recommend one or more of the following tests:
- Digital rectal exam. The doctor or nurse inserts a gloved, lubricated finger into the rectum to feel for abnormalities.
- Barium enema. Also known as a lower gastrointestinal series, this imaging test involves filling the large intestine with barium sulfate, a white liquid that shows up well on X-rays.
- Stool guaiac test. Also known as a fecal occult blood test, this noninvasive test detects hidden blood in the stool. This blood may come from anywhere along the digestive tract. Invisible blood in the stool is often the first – and in many cases, the only – warning sign that a person has colorectal cancer.
- Sigmoidoscopy. This procedure allows doctors to examine the inside of your rectum and lower colon using a flexible endoscope. They may remove any polyps or abnormal tissue for examination under a microscope.
- Colonoscopy. This procedure allows doctors to examine the inside your rectum and your entire colon, removing any polyps or abnormal tissue for examination under a microscope.
- Polypectomy. This is the removal of polyps during a sigmoidoscopy or colonoscopy and analyzing them to see if they are cancerous.
- Biopsy. To make a diagnosis, a small amount of tissue from the suspicious area is removed for microscopic examination by a pathologist.
Staging of rectal cancer
If you are diagnosed with rectal cancer, your doctor needs to determine the stage, or extent, of your disease. Staging is a careful process to assess whether the cancer has spread and, if so, to which parts of the body. This information helps your doctor design the most effective treatment plan for your condition. Additional tests – in particular, an endorectal ultrasound or MRI scan – may be performed to help determine the stage.
The stages of rectal cancer are:
- Stage 0. This is the earliest stage and means the cancer is only in the rectum's innermost lining.
- Stage 1. The cancer involves more of the rectum's inner wall.
- Stage 2. The cancer has spread outside the rectum to nearby tissue but not to lymph nodes. (Lymph nodes are small, bean-shaped structures that are part of the body's immune system.)
- Stage 3. The cancer has spread to nearby lymph nodes but not to other parts of the body.
- Stage 4. The cancer has spread to other parts of the body. Rectal cancer tends to spread to the liver and lungs.
- Recurrent. Recurrent cancer is cancer that has come back after treatment. The disease may recur in the rectum or another part of the body.
Treatment of rectal cancer
Treatment for rectal cancer may include surgery, radiation therapy or chemotherapy – or it may be a combination of these approaches.
Surgery for rectal cancer
Surgery is the main treatment for all stages of rectal cancer, although it's often combined with radiation, chemotherapy or both.
Depending on the tumor's location, stage and size, your surgeon will remove it with one of the following methods:
- Local excision. This surgical approach is used for very early cancers. It involves inserting a colonoscope (a thin lighted tube) through the anus and into the rectum to remove the cancer, rather than making a cut through the abdominal wall. If the cancer is in a polyp, the procedure is called a polypectomy.
- Resection and anastomosis. This approach is used for larger and more advanced cancers. A resection involves removing the portion of the rectum containing the cancer, as well as the fatty tissue that surrounds the rectum and contains lymph nodes. It's followed by a procedure called an anastomosis in which the colon is sewn to the remaining rectum or the anus in order to maintain a passageway.
- Resection and colostomy. This approach is used when the rectum cannot be sewn back together. A colostomy involves creating a stoma, an opening to the outside of the body that will allow waste to pass into a collection bag. The colostomy may be temporary. If the entire rectum is removed, it's permanent.
In some cases, we can remove the cancer using robotic surgery, a minimally invasive computer-supported system that enhances precision.
Radiation therapy for rectal cancer
Radiation therapy is the use of X-rays or other high-energy rays to kill cancer cells and shrink tumors. The radiation may be delivered by a machine outside the body (external beam radiation therapy) or by radioactive materials inserted through thin plastic tubes into the intestinal area (internal radiation therapy). Radiation can be used alone or in addition to surgery and chemotherapy.
Radiation therapy may be used after surgery to kill any remaining cancer cells or before surgery to shrink the tumor. Radiation also can be used to prevent cancer from coming back to the area where it started or to relieve symptoms of advanced cancer.
Chemotherapy for rectal cancer
Chemotherapy uses drugs to kill cancer cells. Chemotherapy may be taken as pills or given intravenously (IV – that is, through a vein). For IV administration, we may place a catheter (a thin tube) that will stay in the vein over a period of weeks while a small pump administers the chemo drug. If your cancer has spread, chemotherapy may be injected directly into the artery supplying the affected part of the body.
Chemotherapy is called a systemic treatment, which means that the drug enters the bloodstream, travels through the body and can kill cancer cells beyond the rectum.
If your surgeon removes all visible cancer during the operation, you may be given chemotherapy after surgery to kill any remaining cancer cells. Chemotherapy after surgery, when you have no detectable cancer cells, is called adjuvant chemotherapy.
Immunotherapy for rectal cancer
Immunotherapy, also call biological therapy, aims to make your body's immune system fight your cancer. Materials made by the body or in a laboratory are used to boost, direct or restore your natural defenses against disease.
Radiofrequency ablation for rectal cancer
Radiofrequency ablation involves using a special probe with tiny electrodes to kill cancer cells. The probe is inserted through an incision in the abdominal wall or directly into the skin, using local anesthesia.
Cryosurgery for rectal cancer
This treatment uses an instrument to freeze and destroy abnormal tissue.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.
More treatment info
-
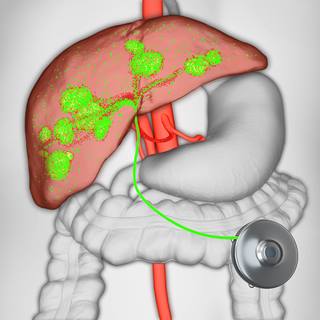
Hepatic Artery Infusion Pump
This implanted pump delivers chemotherapy directly to liver tumors, providing an effective treatment option for metastatic colon or bile duct cancer.
Learn more -
Transanal Endoscopic Microsurgery (TEM)
Surgeons can remove certain non-cancerous and early stage rectal cancers through a minimally invasive procedure.
Learn more -

Virtual Colonoscopy
The procedure is equally effective, less invasive and faster than a standard colonoscopy screening for colon cancer.
Learn more
Recommended reading
Where to get care (4)
Related clinics (4)

Osher Center for Integrative Health
 2
2