Pancreatic Cancer
Overview
The pancreas is an oblong organ, about six inches long, located in the upper abdomen. It has two major functions: The first is to produce digestive enzymes – proteins that help digest food into the small intestine. Cells that perform this function make up the exocrine pancreas.
The second major function is to produce hormones that are secreted into the blood. These cells make up the endocrine pancreas.
Endocrine pancreas
The endocrine pancreas is made up of specialized cells, referred to as islets of Langerhans, that produce hormones. The most important hormone produced is insulin that helps control sugar in the blood.
Cancers that begin in islet cells are called islet cell tumors or pancreatic neuroendocrine tumors. These tumors are rare and may produce hormones that cause very low or very high blood sugars or symptoms such as stomach pain and severe diarrhea.
Exocrine pancreas
The exocrine pancreas is made up of ducts and acini, which are small pockets at the end of the ducts. Cells lining the ducts are the most likely to develop cancer, called ductal adenocarcinomas, the most common type of pancreatic cancer.
These two types of tumors are treated very differently.
At UCSF, we have specialists who conduct research on both types of pancreatic cancers. We have one of the few pancreas cancer research programs in the nation with a team dedicated to learning more about these tumors and developing better treatments.
Risk factors
Although the cause of pancreatic cancer is unknown, risk factors have been identified that increase a person's chance of developing the disease. These include:
- Smoking. People who smoke cigarettes are two to three times more likely to develop pancreatic cancer than non-smokers.
- Age. The risk of pancreatic cancer increases with age. People over the age of 60 are more commonly diagnosed with the disease.
- Race. African Americans are more likely than Asians, Hispanics and whites to develop pancreatic cancer.
- Chronic pancreatitis. A history of chronic pancreatitis may increase the likelihood of developing pancreatic cancer.
- Diabetes. Some people with diabetes are more commonly affected by pancreatic cancer. Diabetes may also be a complication or an early sign of pancreatic cancer. .
- Diet. A diet high in fats, especially processed red meats, may increase the chance of developing pancreatic cancer.
- Weight. Overweight people are more likely than others to develop pancreatic cancer.
Genetics
While most cases of pancreatic cancer don't run in families, inherited conditions may increase the chance of developing pancreatic cancer.
About 5 percent to 10 percent of pancreatic cancers are considered hereditary, or related to a specific genetic mutation. Pancreatic cancer is considered to run in a family when two or more first-degree relatives – such as parents, siblings or children – have the condition. This is sometimes referred to as familial pancreatic cancer (FPC). If a person has a first-degree relative with pancreatic cancer, his or her risk is significantly greater than the average person's.
An increased risk also has been associated with a number of genetic syndromes including hereditary breast, ovarian and colon cancer and a serious type of skin cancer called familial atypical multiple mole syndrome (FAMMM).
Our approach to pancreatic cancer
In the past, pancreatic cancer was often caught at a late stage, making it difficult to treat. UCSF is using new technology that helps doctors diagnose pancreatic cancer earlier, and also helps us detect cysts, tumors and other abnormal tissue that could lead to cancer if left untreated. Our advanced, customized treatments and follow-up care are saving more lives.
As home to one of the few dedicated pancreatic cancer research programs in the U.S., we're at the forefront of developing better therapies. Interested patients may have the opportunity to join clinical trials.
Awards & recognition
-

Among the top hospitals in the nation
-

Best in Northern California and No. 7 in the nation for cancer care
-

Designated comprehensive cancer center
Signs & symptoms
Pancreatic cancer often is called a "silent" disease because it typically doesn't cause symptoms early on. The cancer may grow and spread for some time before symptoms develop, which may be so vague that they are initially ignored. For these reasons, pancreatic cancer is hard to detect early. In many cases, the cancer has spread outside the pancreas by the time it is found.
When symptoms appear, their type and severity depend on the location and size of the tumor.
Common symptoms may include:
- Jaundice. If the tumor blocks the bile duct so bile can't flow into the intestines, jaundice may occur, causing the skin and whites of the eyes to turn yellow, the urine to become dark and the stool to turn clay-colored.
- Pain. As the cancer grows and spreads, pain often develops in the upper abdomen and the back. The pain may increase after a person eats or lies down.
- Weight loss. Cancer of the pancreas can also cause unintentional weight loss. This is often due to an inadequate intake of calories because of nausea, vomiting and loss of appetite.
- Digestive problems. Digestive problems may occur if the cancer blocks the pancreatic juices from flowing into the intestines, which help the body break down dietary fats, proteins and carbohydrates. Stools may be different than usual and appear pale, bulky or greasy, float in the toilet, or be particularly foul-smelling.
Diagnosis
It is important to note that pancreatic cancer is not just one disease. There are many types of pancreatic tumors, each with its own unique prognosis and treatment recommendations. Currently, there is no screening exam of proven value for detecting pancreatic cancer in the general population.
In making a diagnosis of pancreatic cancer, your doctor may conduct the following tests.
Medical history and physical examination
A series of tests may be necessary to make a definite diagnosis. Your doctor will first start by asking about your medical history and any physical complaints or symptoms, specifically recent weight loss, pain and changes in appetite, bowel patterns or skin color. The doctor will then complete a thorough physical exam, which will include palpation and observation of the chest and abdomen.
Lab tests
Blood specimens may be collected and less commonly, urine or stool samples. Of particular interest to the doctor is the level of "bilirubin" and "liver enzymes" in a patient's blood, which measures liver and pancreas function.
Another blood test commonly performed is CA19-9 (carbohydrate antigen 19-9). CA19-9 is referred to as a "tumor marker," which is a chemical substance in the body that may be found at higher levels if cancer is present.
An elevated CA 19-9 test by itself is not used to make the diagnosis of pancreatic cancer, as it can be elevated in a variety of other conditions, such as pancreatitis or cirrhosis of the liver, and some people with pancreatic cancer do not show this marker at all.
CA 19-9 can be used as a tool, however, to help evaluate the effectiveness of a cancer therapy by comparing the levels before and during treatment.
Additional diagnostic tests
The following tests may also be conducted to make a definite diagnosis:
- Ultrasound. Ultrasound uses a machine that emits high-frequency sound waves to create images of the organs inside the body. An abdominal ultrasound examines the liver, gallbladder, spleen, pancreas and kidneys, and can help identify abnormal structures or tissue.
- Computed tomography (CT) scan. This is a non-invasive method of examining internal organs that captures a series of thin X-ray images of the inside of the body. CT scans can help detect tumors and determine whether it has spread to other parts of the body, such as the liver. There are different types of CT scans and special techniques that can be done to create more detailed images of the pancreas. At UCSF, we offer a three-dimensional CT scan, often referred to as a "spiral" or "helical" scan, which creates extremely detailed images of the pancreas and nearby blood vessels and structures to help determine treatment decisions.
- Endoscopic ultrasound (EUS). This is a procedure that allows a specially trained doctor, typically a gastroenterologist, to view the esophagus, stomach and the first portion of the small intestine, as well as adjacent organs including the liver and pancreas. While the patient sleeps, a thin, flexible tube called an endoscope is passed through the mouth into the stomach and small intestine. On the end of the tube is an ultrasound probe that emits sound waves that create images of the abdominal organs. If unusual masses are detected, the doctor may collect a specimen of tissue at the time of the procedure during a biopsy. The use of EUS can decrease the likelihood that a patient will need to go to the operating room for surgery.
- Endoscopic retrograde cholangiopancreatography (ERCP). This procedure uses an endoscope – a long, flexible, lighted tube connected to a computer and TV monitor. Your doctor will guide the endoscope through your stomach and into the small intestine. ERCP combines two imaging techniques: "endoscopy," the direct visualization of internal structures and "fluoroscopy," a live action X-ray method. These two techniques allow the doctor to view images of the liver, gall bladder and pancreas ducts, which can help detect a narrowed or blocked duct. Further tests, such as a biopsy, can pinpoint the cause of a narrowed or blocked duct. If a duct is narrowed or blocked by a tumor, a plastic or metallic stent can be placed across the blockage. The stent is designed to expand and reopen the duct to allow bile juices to flow freely.
- Magnetic resonance cholangiopancreatography (MRCP). MRCP uses radio waves and a powerful magnet linked to a computer to visualize the biliary and pancreatic ducts in a non-invasive manner. These pictures can show the difference between normal and diseased tissue and can also detect bile duct obstruction. MRCP may be performed in patients who cannot have an endoscopic retrograde cholangiopancreatography (ERCP) or may also prevent unnecessary invasive procedures.
- Biopsy. A biopsy allows a doctor to collect a small amount of tissue. A pathologist then uses a microscope to examine the tissue and identify the types of cells collected. Tissue can be collected at the time of an endoscopic ultrasound or endoscopic retrograde cholangiopancreatography. A biopsy also can be performed under guidance of a CT scan. If necessary, a biopsy can be performed at the time of open surgery of the abdomen. There are two methods frequently used to collect tissue for a biopsy. A fine needle aspiration (FNA) utilizes a very narrow needle. A core needle biopsy uses a larger needle. Both methods have advantages and risks. If cancer is suspected to have spread, or metastasized, it is preferable to biopsy the tumor than the pancreas itself. A specially trained doctor will determine the best method to use. It is also important to note that if all of your other test results suggest cancer, you may not need a biopsy before you have treatment.
Staging
If you are diagnosed with pancreatic cancer, your doctor will evaluate the stage or extent of your disease. Staging is a careful attempt to determine the size and location of the cancer and whether it has spread to other parts of the body.
The stage of a cancer is a description of the extent of a cancer at a specific point in time. This information helps your doctor develop the best and most effective treatment plan for your condition. The stage may be determined at the time of diagnosis or after more tests are performed.
There are two forms of a staging system for cancer:
- Clinical staging involves a doctor's exam and imaging tests such as a computed tomography (CT) scan.
- Pathologic staging depends on findings from surgery. However, most patients with pancreatic cancer do not have surgery. Doctors will develop a treatment plan according to the extent of disease.
Stages of pancreatic cancer
- Localized and resectable. The cancer is confined to the pancreas and is resectable, meaning that in most cases, it can be surgically removed. After surgical removal, most patients receive additional treatment such as cancer drugs or radiation therapy.
- Locally advanced and unresectable. When cancer cannot be removed entirely by surgery, it is termed unresectable. Although the cancer has not yet spread to distant organs, the involvement of local structures, usually major blood vessels, make surgical removal technically impossible. In some cases, surgery might be done to relieve symptoms or problems caused by the cancer. Treatment generally includes drugs and sometimes radiation.
- Metastatic. The cancer has spread to distant organs. In this case, surgery might be done to relieve symptoms or problems caused by the cancer. More often, drug therapy is used.
Treatments
There are different treatments available for patients with pancreatic cancer, including surgery, radiation therapy and drug therapy. Your doctor will use the following criteria to develop a treatment plan:
- Your overall health and well being and preferences regarding treatment
- Whether or not the cancer can be removed by surgery
- Whether the cancer has just been diagnosed or has recurred, which means that it has come back
Surgery
About 15 percent to 20 percent of patients with pancreatic cancer are diagnosed early enough that their tumor can be removed surgically. Typically, however, only smaller tumors are surgically removed and even then, cancer often returns.
Pancreatic cancer surgery is a complex procedure. Studies have found that patients do better overall when their surgery is performed at a medical center with a high volume of these surgical procedures. Although the definition of high volume varies by study, UCSF surgeons perform major pancreatic surgeries at a rate well above that which is considered high volume. We are among the most experienced and successful in performing this exacting surgery to treat pancreatic cancer.
Surgery may be performed to remove all or part of the pancreas and nearby tissue. Surgery is also used to try to minimize the complications caused by pancreatic cancer. The kind of surgery recommended depends on your type of cancer, location of the tumor, your symptoms, whether the cancer involves other organs and whether the cancer can be completely removed. It is important to note that even after having surgery, the cancer often recurs.
If imaging studies show that all of your tumor may be potentially removed, one of the following procedures may be performed:
- Whipple procedure (pancreaticoduodenectomy). This is the most commonly performed surgery used to remove tumors of the pancreas. The surgeon removes the head of the pancreas, and sometimes the body of the pancreas. The bottom section of the stomach, parts of the small intestine, gallbladder, a portion of the bile duct and lymph nodes near the pancreas are also removed. The remaining tail of the pancreas and bile duct is reattached to the small intestine so that bile from the liver can flow into the small intestine.
- Robotic Whipple procedure. This is a minimally invasive alternative to the traditional Whipple procedure for pancreatic cancer. Instead of operating through one large incision, the surgeon makes several small incisions and, guided by a tiny camera, uses robotic arms and specialized instruments to remove the affected tissues and organs.
- Distal pancreatectomy. The surgeon removes the body and the tail of the pancreas. The spleen is also often removed.
- Total pancreatectomy. In this procedure, the entire pancreas, duodenum, bile duct, gallbladder, spleen and nearby lymph nodes are removed. While a total pancreatectomy is usually effective in removing the cancer, it induces permanent diabetes, requiring patients to take insulin shots or use an insulin pump for the rest of their lives. This is because the pancreas contains Islets of Langerhans, also known as islets or islet cells, which secrete insulin to regulate the body's blood sugar levels. In some cases, the cancer cannot be completely removed and other surgeries and procedures can be considered to alleviate symptoms.
- Biliary bypass. This surgery is performed if cancer blocks the free flow of bile juice through the bile ducts. This obstruction can cause pain, infection, digestive problems and jaundice, a yellowing of the eyes and skin. Biliary bypass involves rerouting the flow of bile from the common bile duct directly into the small intestine, bypassing the pancreas.
- Biliary stent. This procedure may be performed if cancer blocks the flow of bile in the bile ducts. It involves placing a stent – a small thin plastic or metal tube – to help keep the bile duct open. A biliary stent can be placed either during an endoscopic retrograde cholangiopancreatography (ERCP) or via a route through the skin, into the liver or common bile duct. The stents may be changed or cleared periodically due to buildup from the bile.
- Gastroduodenal stent. Pancreatic tumors may cause an obstruction of the gastric tract, particularly within the duodenum, a part of the small intestine. Symptoms associated with obstruction are severe nausea, vomiting, malnutrition and dehydration. Gastroduodenal stent placement is a minimally invasive technique that can help relieve such symptoms and improve one's quality of life. The procedure is performed in similar fashion to that of the biliary stent described above.
- Gastric bypass. In some cases, the duodenum – the first part of the small intestine – may be blocked by the tumor, causing pain, vomiting and digestive problems. Gastric bypass may be performed to reroute the stomach connection to the duodenum to alleviate symptoms and to allow patients to eat normally.
- Celiac plexus block. Sometimes a celiac plexus block (CPB) or celiac plexus neurolysis (CPN) is performed for pain control. This procedure blocks a group of nerves in the abdomen called the celiac plexus, which can deliver sensations of pain from the abdomen to the brain. CPN involves the injection of an agent, usually alcohol, to permanently destruct nerves. CPB involves the injection of medications such as corticosteroids and numbing medications. This approach usually lasts a few months and is not intended to permanently destroy nerves.
Radiation therapy
Radiation therapy is the use of X-rays or high-energy rays to kill cancer cells and shrink tumors. Radiation is typically delivered by a machine outside the body, called external radiation therapy. Less common, experimental approaches use materials called radioisotopes delivered inside the body through intravenous or local injection.
The use of radiation therapy depends on a number of factors including tumor location, size, organ involvement and previous treatments. Radiation can be used alone or in addition to surgery and chemotherapy. Newer approaches, such as stereotactic radiosurgery with a machine called a CyberKnife are also being explored.
Cancer drug therapy
Cancer drugs may be taken by mouth as a pill or may be put into the body by a needle in the vein. Cancer drugs are a systemic treatment, which means that they enter the bloodstream and travel throughout the body. They attempt to wipe out any cancer cells after surgery or to control disease when surgery is not feasible.
These medications are sometimes taken at the same time as radiation therapy to try to achieve a better result. Drug therapy aims to control cancer, prevent complications and help people live longer and feel better.
Sometimes newer cancer drugs are referred to as targeted therapy. Targeted therapy is a general term that typically refers to a new class of drugs or agents that are designed to target specific parts or pathways that regulate cancer cell growth. In addition, doctors hope that targeted therapies will be less likely to cause unpleasant side effects by minimizing damage to normal cells. This is an area of research that is ever-growing; our pancreatic scientists and doctors are increasingly involved in research studies and clinical trials developing targeted therapies.
Clinical trials
UCSF researchers are at the forefront of studying new therapies for pancreatic cancer. Patients may participate in clinical trials to test new therapies for pancreatic cancer. Clinical trials are experiments designed to improve existing treatment or to test the safety and effectiveness of new treatments.
Participation in a clinical trial is voluntary. Prior to enrollment in a clinical trial, patients are given a document called a consent form that explains the goals of the trial, the therapy to be used, risks and benefits and any associated costs, if applicable. There are a number of mechanisms in place, both legal and ethical, to protect the rights and safety of clinical trial volunteers.
Clinical trials can allow patients access to newer, unproven treatments. They also allow doctor and researchers access to data collected from clinical trial volunteers. Clinical trials will lead to better cancer treatments.
View our current list of pancreatic cancer clinical trials.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.
More treatment info
-
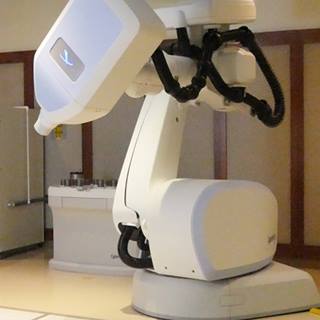
CyberKnife
Radiosurgery minimizes radiation exposure to healthy tissue surrounding a tumor and offers rapid relief from pain and other symptoms.
Learn more -

Robotic Whipple Surgery
UCSF Health is the first San Francisco hospital to offer this minimally invasive treatment for pancreatic cancer.
Learn more
Recommended reading
Where to get care (5)
Related clinics (4)

Osher Center for Integrative Health
 2
2