Diabetes Mellitus
Overview
Diabetes mellitus has become an epidemic in the United States with about 1 million people over age 20 diagnosed with the condition each year. About 17 million people, or 6 percent of the U.S. population, have diabetes mellitus, a disease in which the body doesn't produce or properly use insulin, a hormone produced in the pancreas that converts sugar into energy.
Diabetes, the sixth leading cause of death in the United States, can cause serious health complications such as blindness, kidney failure, nerve damage and the need for lower-extremity amputations. In addition, diabetes is a major risk factor for cardiovascular disease, dramatically increasing the risk for heart disease and stroke.
Types of diabetes
There are three main types of diabetes:
Type 1 diabetes. About 5 to 10 percent of those with diabetes have type 1 diabetes. It's an autoimmune disease, meaning the body's own immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas. Patients with type 1 diabetes have very little or no insulin, and must take insulin everyday. Although the condition can appear at any age, typically it's diagnosed in children and young adults, which is why it was previously called juvenile diabetes.
Type 2 diabetes. Accounting for 90 to 95 percent of those with diabetes, type 2 is the most common form. Usually, it's diagnosed in adults over age 40 and 80 percent of those with type 2 diabetes are overweight. Because of the increase in obesity, type 2 diabetes is being diagnosed at younger ages, including in children. Initially in type 2 diabetes, insulin is produced, but the insulin doesn't function properly, leading to a condition called insulin resistance. Eventually, most people with type 2 diabetes suffer from decreased insulin production.
Gestational diabetes. Gestational diabetes develops during pregnancy. It occurs more often in African Americans, Native Americans, Latinos and people with a family history of diabetes. Typically, it disappears after delivery, although the condition is associated with an increased risk of developing diabetes later in life.
Our approach to diabetes mellitus
UCSF offers comprehensive diabetes care founded on our cutting-edge research program. As a federally recognized diabetes research center, we strive to quickly translate laboratory discoveries into improved treatments and even cures. We are one of the few medical centers in the nation that can perform islet transplants for type 1 diabetes, providing a temporary cure that allows many recipients to live diabetes free for the first time in their lives. U.S. News & World Report consistently ranks UCSF Medical Center among the top five hospitals in the country for diabetes care.
We complement medical care with a variety of classes and workshops covering topics such as healthful cooking and exercise, as well as a support network for people living with diabetes. Our mission is to empower patients with the tools and information they need to lead full, healthy lives.
Explore what we do
Amputation prevention center offers hope for tough cases
For patients with diabetes who are at risk of losing limbs, our specialists in numerous fields draw on groundbreaking research to offer cutting-edge care.
Awards & recognition
-

Among the top hospitals in the nation
-

One of the nation’s best for diabetes care & endocrinology
-

Rated high-performing hospital for diabetes care
Signs & symptoms
If you think that you have diabetes, visit your doctor immediately for a definite diagnosis. Common symptoms include the following:
- Frequent urination
- Excessive thirst
- Unexplained weight loss
- Extreme hunger
- Sudden vision changes
- Tingling or numbness in the hands or feet
- Feeling very tired much of the time
- Very dry skin
- Sores that are slow to heal
- More infections than usual
Some people may experience only a few symptoms that are listed above. About 50 percent of people with type 2 diabetes don't experience any symptoms and don't know they have the disease.
Diagnosis
Your doctor will first ask about your medical history and perform a physical examination to check for symptoms of diabetes and high blood sugar. Diabetes usually is diagnosed with the following tests that measure the glucose levels in your blood:
- Fasting plasma glucose test. This is the standard test for diagnosing type 1 and type 2 diabetes. You must not eat or drink anything for at least eight hours prior to this simple test in which blood is drawn to check your sugar levels. A diagnosis of diabetes will be made if you have a fasting blood sugar level of 126 milligrams per deciliter or higher on two separate days.
- Other tests. Diabetes also may be diagnosed based on a random high glucose level of 200mg/dl and symptoms of the disease. Your doctor may wish to perform an oral glucose tolerance test, which is the traditional test for diabetes mellitus.
Treatments
The goal of diabetes management is to keep blood glucose levels as close to normal as safely possible. Since diabetes may greatly increase risk for heart disease and peripheral artery disease, measures to control blood pressure and cholesterol levels are an essential part of diabetes treatment as well.
People with diabetes must take responsibility for their day-to-day care. This includes monitoring blood glucose levels, dietary management, maintaining physical activity, keeping weight and stress under control, monitoring oral medications and, if required, insulin use via injections or pump. To help patients achieve this, UCSF's Diabetes Teaching Center offers self-management educational programs that emphasize individualized diabetes care. The program enables patients to make more consistent and appropriate adjustments in their therapy and lifestyle.
Dietary management and physical activity
Modifying eating habits and increasing physical activity are typically the first steps toward reducing blood sugar levels. At UCSF Medical Center, all patients work with their doctor and certified dietician to develop a dietary plan. Our Teaching Center conducts workshops that provide patients with information on food nutrient content, healthy cooking and exercise.
Insulin therapy
People with type 1 diabetes require multiple insulin injections each day to maintain safe insulin levels. Insulin is often required to treat type 2 diabetes too. Using an insulin pump is an alternative to injections. The pump is about the size of a pager and is usually worn on your belt. Insulin is delivered through a small tube (catheter) that is placed under the skin (usually in the abdomen).
There are four major types of insulin:
- Rapid-acting
- Short-acting
- Intermediate-acting
- Long-acting
Your doctor will determine your dose and how often you need to take insulin. There is no standard insulin dose as it depends on factors such as your body weight, when you eat, how often you exercise and how much insulin your body produces.
Oral medications
Sometimes blood sugar levels remain high in people with type 2 diabetes even though they eat in a healthy manner and exercise. When this happens, medications taken in pill form may be prescribed. The medications work in several different ways. These include improve the effectiveness of the body's natural insulin, reduce blood sugar production, increase insulin production and inhibit blood sugar absorption. Oral diabetes medications are sometimes taken in combination with insulin.
Learn more about our Diabetes Education Online and classes and workshops at the UCSF Diabetes Center.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.
More treatment info
-
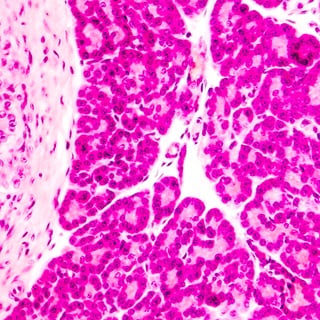
Islet Transplant for Type I Diabetes
Type 1 diabetes can be temporarily reversed with islet cells from a donor.
Learn more -

Kidney Transplant
Learn what to expect during a kidney transplant evaluation and how the procedure is performed.
Learn more -

Pancreas Transplant
By restoring insulin production, a successful pancreas transplant can improve health issues caused by type 1 diabetes.
Learn more













