Fibroids
Overview
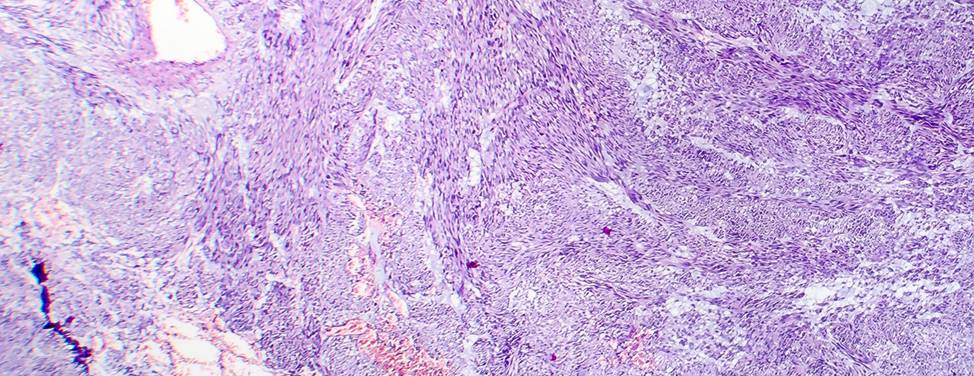
Fibroids are round growths that develop in the uterus. They are almost always benign, or non-cancerous. Fibroids range in size from as small as a pea to as large as a melon. They are also called leiomyomas or myomas.
Fibroids are very common, affecting an estimated 20 to 50 percent of all women. They are most likely to affect women in their 30s and 40s, and for reasons we don't understand, occur more frequently in African-Americans. Many women with fibroids have family members who also have them.
Some fibroids grow steadily during the reproductive years, while others stay the same size for many years. All fibroids should stop growing after menopause. If your fibroids grow after menopause, you should consult your doctor.
Usually, fibroids cause no symptoms and don't require treatment. But if symptoms occur, you should seek medical attention.
Types of fibroids
Fibroids can grow in different parts of the uterus:
- Pedunculated fibroids are attached to the uterine wall by stalks.
- Subserosal fibroids extend outward from the uterine wall.
- Submucosal fibroids expand from the uterine wall into the uterine cavity.
- Intramural fibroids develop within the uterine wall.
Different types of fibroids are associated with different symptoms. For example, submucosal fibroids typically cause heavy periods. In contrast, subserosal fibroids are more likely to push against the bladder, causing frequent urination.
Causes of fibroids
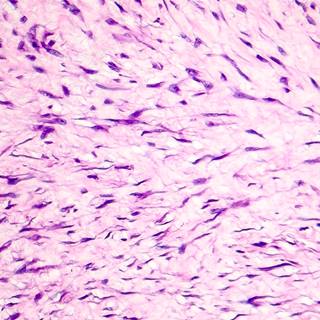
Doctors and medical researchers do not know what causes fibroids to develop. There is evidence that the female hormones, estrogen and progesterone, can make them grow. During pregnancy, when the hormone levels are high, fibroids tend to increase in size. After menopause, when the hormone levels are low, fibroids stop growing and may become smaller.
Our approach to fibroids
There are many effective ways to treat uterine fibroids. UCSF offers a wide range of treatments, including innovative and minimally invasive surgical techniques. When needed, we coordinate care with other experts at UCSF, such as fertility doctors and obstetricians who specialize in high-risk pregnancy.
The best treatment choice for each woman depends on personal preference as well as the size and location of her fibroids. We believe that empowering women with knowledge is an important part of the healing process, and encourage each patient to participate in choosing the best treatment option for her.
Awards & recognition
-

Among the top hospitals in the nation
Signs & symptoms
Symptoms of fibroids may include:
- Heavy vaginal bleeding. Excessively heavy or prolonged menstrual bleeding is a common symptom. Women describe soaking through sanitary protection in less than an hour, passing blood clots and being unable to leave the house during the heaviest day of flow. As a result, some women develop anemia, also known as a low blood count. Anemia can cause fatigue, headaches and lightheadedness. If heavy bleeding interferes with your everyday activities or if you develop anemia, you should see your doctor to discuss fibroid treatment options.
- Pelvic discomfort. Women with large fibroids may feel heaviness or pressure in their lower abdomen or pelvis. Often this is described as a vague discomfort rather than a sharp pain. Sometimes, the enlarged uterus makes it difficult to lie face down, bend over or exercise without discomfort.
- Pelvic pain. A less common symptom is acute, severe pain. This occurs when a fibroid goes through a process called degeneration. Usually, the pain is localized to a specific spot and improves on its own within two to four weeks. Using a pain reliever, such as ibuprofen, can decrease the pain significantly. However, chronic pelvic pain can also occur. This type of pain is usually mild but persistent and confined to a specific area.
- Bladder problems. The most common bladder symptom is needing to urinate frequently. A woman may wake up several times during the night to empty her bladder. Occasionally, women are unable to urinate despite a full bladder. These symptoms are caused by fibroids pressing against the bladder, reducing its capacity for holding urine or blocking the outflow of urine. Treatment for bladder problems can provide great relief.
- Low back pain. Rarely, fibroids press against the muscles and nerves of the lower back and cause back pain. A large fibroid on the back surface of the uterus is more likely to cause back pain than a small fibroid within the uterine wall. Because back pain is so common, it is important to look for other causes of the pain before attributing it to fibroids.
- Rectal pressure. Fibroids also can press against the rectum and cause a sensation of rectal fullness, difficulty having a bowel movement or pain with bowel movements. Sometimes, fibroids can lead to the development of a hemorrhoid.
- Discomfort or pain with sexual intercourse. Fibroids can make sexual intercourse painful or uncomfortable. The pain may occur only in specific positions or during certain times of the menstrual cycle. Discomfort during intercourse is a significant issue. If your doctor doesn't ask you about this symptom, make sure you mention it.
Diagnosis
Usually, fibroids are found during a routine gynecologic visit with a pelvic examination. A pelvic exam allows the doctor to feel the size and shape of the uterus; if it is enlarged or irregularly shaped, fibroids may be present. Or, you may notice new symptoms and inform your doctor.
If your doctor thinks you may have fibroids after performing the exam, there are several tests that can confirm the diagnosis. The first is usually an ultrasound. The other tests are more specialized and are only performed if needed to guide treatment options. Below is a brief description of each type of exam.
- Ultrasound. Many women are familiar with ultrasound from pregnancy, when it is used to evaluate the growing fetus. Ultrasound is also a safe and reliable way to look for fibroids. In the test, sound waves are used to create a picture of the uterus and ovaries. Ultrasound does not use radiation.
The procedure takes between 30 to 60 minutes. The initial portion of the exam is performed with the transducer on the abdomen. Conducting gel is placed on the skin, which feels wet and cool. The transducer is moved around as the technologist takes pictures of the uterus and ovaries.
The second portion of the exam is performed internally. You will need to empty your bladder first. A special ultrasound probe will then be placed in the vagina. It is usually not painful and is inserted like a tampon. Close-up pictures are then taken of the uterus, endometrium (the lining of the uterus) and ovaries. The radiologist reviews all the pictures and will report the results to your doctor. - Saline Hysterosonography. This is also an ultrasound procedure which uses no radiation. The exam helps us better visualize the inside of the uterus and endometrium. Submucosal fibroids and polyps can easily be identified by this method.
The exam takes about half an hour. It is often performed right after the woman finishes her menstrual period. A small catheter is inserted through the cervix and a small balloon is inflated to hold it in place. Sterile saline is injected into the uterus and ultrasound pictures are taken. During the procedure you may experience some cramping, similar to menstrual cramps. The cramps may last for a short time after the procedure – this is normal. - Magnetic Resonance Imaging (MRI). MRI is more expensive than ultrasound but gives doctors a reproducible, detailed picture of the number, size and exact location of the fibroids. Not all women with fibroids need an MRI. All patients that are being evaluated for a uterine artery embolization will get one, however. MRI uses a large, special magnet to take pictures of the body. The test does not use radiation.
The exam takes about 45 to 60 minutes, during which time you are asked to remain still. Before the study begins, an intravenous (IV) line is placed in your arm. You then lie down on a moveable bed. The big magnet is shaped like a donut, through which this moving bed passes. Contrast material is injected through the IV and pictures are taken of the pelvic area. These images will be reviewed by a radiologist who will report the findings to your doctor. - Hysteroscopy. Diagnostic hysteroscopy is another procedure for seeing inside the uterus. The test can be performed in a doctor's office or in an operating room. Submucosal fibroids and polyps can be easily identified with this test. It takes 30 minutes to complete.
For the test, you will lie on your back with your feet in gynecology stirrups. A speculum is placed in the vagina. A long, slender telescope, called a hysteroscope, is gently inserted through the cervix into the uterine cavity. For ideal viewing, sterile saline or CO2 gas is introduced through the hysteroscope to inflate the cavity. Images of the lining of the uterus, the openings of the fallopian tubes, polyps and submucus fibroids are displayed on a TV monitor. Women experience mild cramps during the procedure. Taking ibuprofen (Advil, Motrin) one hour before the procedure can alleviate the discomfort.
Treatments
Treatment for fibroids can range from no treatment at all to surgery. Unless fibroids are causing excessive bleeding, discomfort or bladder problems, treatment usually isn't necessary.
If you have fibroids, you should be evaluated periodically to review symptoms, and to monitor the fibroid and uterus size with abdominal and pelvic examinations. If you don't have symptoms, routine pelvic ultrasounds have very little benefit. Fibroids are likely to grow each year until menopause, but this isn't an indication that you need treatment, unless the change is accompanied by disabling symptoms.
The following are treatment options for fibroids:
Medications
Currently, the medications available for fibroids can temporarily improve symptoms but do not make the fibroids go away. For women with heavy bleeding, it is worth trying medication before undergoing a surgical procedure. Women with pressure symptoms caused by large fibroids won't benefit from any medicines currently available.
There are several promising new drugs on the horizon that will treat the fibroids themselves, not just the symptoms.
Contraceptive pills and progestational agents
Women with heavy menstrual periods and fibroids are often prescribed hormonal medications to try to reduce bleeding and regulate the menstrual cycle. These medications will not shrink fibroids or make them grow at a faster rate.
If the medication has not improved your bleeding after three months, consult your doctor. Women over the age of 35 who smoke should not use oral contraceptives.
GnRH agonists (Lupron)
GnRH agonists are a class of medications that temporarily shrink fibroids and stop heavy bleeding by blocking production of the female hormone, estrogen. Lupron is the most well known of these drugs. Although Lupron can improve fibroid symptoms, it causes unpleasant menopausal symptoms such as hot flashes. Long-term use can cause bone loss.
Lupron is recommended only for very specific cases. It may be recommended if you have heavy bleeding and serious anemia, and would need a blood transfusion during fibroid surgery. If you take Lupron for two to three months before surgery, your periods may temporarily stop and eliminate the need for a blood transfusion. Lupron also may be recommended if you have very large fibroids – greater than 10 to 12 centimeters – prior to fibroid surgery. Lupron should not be used solely to shrink fibroids unless surgery is planned, because fibroids will re-grow to their original size as soon as you stop taking Lupron.
Intrauterine devices (IUD)
Although IUDs are typically used to prevent pregnancy, they have other benefits as well. An IUD that releases a small amount of hormone into the uterine cavity can decrease bleeding caused by fibroids.
An IUD can be inserted during a routine office appointment.
Myomectomy
A myomectomy is an operation to remove fibroids while preserving the uterus. For women who have fibroid symptoms and want to have children in the future, myomectomy is the best treatment option.
Myomectomy is very effective, but fibroids can re-grow. The younger you are and the more fibroids you have at the time of myomectomy, the more likely you are to develop fibroids again in the future. Women nearing menopause are the least likely to have recurring problems from fibroids after a myomectomy.
A myomectomy can be performed several different ways. Depending on the size, number and location of your fibroids, you may be eligible for an abdominal myomectomy, a laparoscopic myomectomy or a hysteroscopic myomectomy.
- Abdominal myomectomy. During this operation, an incision is made through the skin on the lower abdomen (a "bikini cut"). The fibroids are removed from the wall of the uterus, and the uterine muscle is sewn back together using several layers of stitches. You will be asleep for the procedure. Most women spend two nights in the hospital and four to six weeks recovering at home.
- Laparoscopic myomectomy. In a laparascopic myomectomy, four one-centimeter incisions are made in the lower abdomen: one at the belly button, one below the bikini line near the pubic hair, and one near each hip. The abdominal cavity is filled with carbon dioxide gas. A thin, lighted telescope is placed through an incision so the doctors can see the ovaries, fallopian tubes and uterus. Long instruments, inserted through the other incisions, are used to remove the fibroids. The uterine muscle is then sewn back together, the gas is released and the skin incisions are closed. You will be asleep for the procedure. The recovery is shorter than for an abdominal myomectomy – typically, women spend one night in the hospital and two to four weeks recovering at home.
- Hysteroscopic myomectomy. Only women with submucosal fibroids – fibroids that expand from the uterine wall into the uterine cavity – are eligible for this type of myomectomy. Fibroids located within the uterine wall cannot be removed with this technique. During the procedure, you will lie on your back with your feet in gynecology stirrups. You will most likely be asleep for the procedure. A speculum is placed in the vagina and a long, slender telescope is placed through the cervix into the uterine cavity. The uterine cavity is filled with fluid to lift apart the walls of the uterus. Instruments passed through the hysteroscope are used to shave off the submucosal fibroids. This is an out-patient procedure, and you may go home after several hours of observation in the recovery room. Most women spend one to four days resting at home to recover.
Read more about myomectomy.
Hysterectomy
Hysterectomy is a major surgical procedure in which the uterus is removed. Many women choose hysterectomy to definitively resolve their fibroid symptoms. After hysterectomy, menstrual bleeding stops, pelvic pressure is relieved, frequent urination improves and new fibroids cannot grow. A woman can no longer become pregnant after a hysterectomy.
The ovaries are not necessarily removed during a hysterectomy. Generally, if a woman is in menopause or close to menopause, the ovaries are removed. The ovaries may also be removed if they look abnormal or if the patient wants to decrease her chance of developing ovarian cancer later in life. In pre-menopausal women, removal of the ovaries can cause hot flashes, vaginal dryness and other symptoms. You should discuss the pros and cons of ovarian removal with your doctor.
There are several hysterectomy surgical approaches: a vaginal hysterectomy, an abdominal hysterectomy and a laparoscopic hysterectomy. The choice of procedure will depend on the size of the uterus and several other factors.
- Vaginal hysterectomy. A vaginal hysterectomy is performed by removing the uterus through the vagina, rather than through an incision on the abdomen. To be eligible for a vaginal hysterectomy, your uterus cannot be too large. You will be asleep for the procedure. Most women stay two nights in the hospital. The recovery involves significant pain for 24 hours and mild pain for 10 days. Full recovery usually takes four weeks.
- Abdominal hysterectomy. In an abdominal hysterectomy, the uterus is removed through a horizontal incision on the lower abdomen, called a "bikini cut." If the uterus is very large or if there is a scar from an earlier operation, it may be necessary to make a vertical incision instead. A total abdominal hysterectomy means removing the uterus and the cervix. Women who have had abnormal pap smears are usually encouraged to have their cervix removed. A subtotal or supra-cervical hysterectomy means removing only the upper part of the uterus. Women who retain their cervix may have less bladder leakage and vaginal relaxation later in life; however, this has not been scientifically proven. Women who have had a supra-cervical hysterectomy will continue to need periodic pap smears. In addition, some women will have monthly spotting or light bleeding if endometrial glands are still embedded in the cervical tissue. You will be asleep during the procedure. Most women spend three nights in the hospital and six weeks recovering at home. Some women experience a complication that results in a longer recovery time.
- Laparoscopic hysterectomy. This is a new procedure in which the uterus is removed through very small incisions on the lower abdomen. The cervix remains in place. Women with large fibroids or a large uterus may not be candidates for a laparoscopic hysterectomy. In the procedure, four one-centimeter incisions are made in the lower abdomen: one at the belly button, one below the bikini line near the pubic hair, and one near each hip. The abdominal cavity is filled with carbon dioxide gas. A thin, lighted telescope is placed through an incision so the doctors can see the ovaries, fallopian tubes and uterus. Long instruments, inserted through the other incisions, are used to remove the uterus. A special instrument is used to cut the uterus into smaller segments for removal through the small incisions. At the end of the procedure, the gas is released and the skin incisions are closed. You will be asleep during the procedure. Most women spend one night in the hospital and two to four weeks recovering at home.
Read more about hysterectomy.
Uterine artery embolization (UAE)
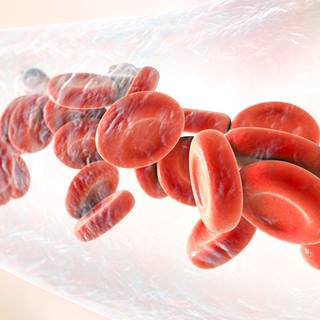
Uterine artery embolization is a relatively new procedure and an alternative to open surgery for fibroids. Embolization is a technique that blocks the blood flow to the fibroid or fibroids, causing them to shrink and die. This also often decreases menstrual bleeding and symptoms of pain, pressure, urinary frequency or constipation.
UAE is performed in a radiology suite rather than an operating room, by an interventional radiologist. An intravenous (IV) line will be placed before beginning the procedure, and you will be sedated. You will remain awake, but sleepy, throughout the procedure.
A needle is placed in an artery in your leg, at the groin crease. A small catheter is then placed into the artery and X-rays are taken of the arteries – a test called an arteriogram – that supply the fibroids. The catheter is then used to select these arteries and slowly inject particles called polyvinyl alcohol, which are the size of a sand grain. The particles block the flow of blood. After the left and right uterine arteries are embolized, another arteriogram is performed to confirm the procedure is complete.
Afterward, you must rest in bed for six hours, lying flat with your leg straight. The amount of pain patients experience varies. The most significant pain usually occurs immediately following the procedure and over the next six hours. Patients usually stay overnight in the hospital, so we can monitor the arterial access site and provide adequate pain control. You will be discharged the next morning. Most women can return to full activity in a week.
When blood flow to the fibroid is blocked, the fibroid gets no oxygen and will begin to die. This process happens over days to months. During this time the fibroid shrinks by about 40 to 50 percent and the uterus by about 30 to 40 percent. Our experience and the scientific literature suggest that symptoms will improve in 80 to 90 percent of patients. For some, UAE is ineffective. Serious complications occur in less then four percent of patients.
Read more about uterine artery embolization.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.
More treatment info
-

Hysterectomy
Several hysterectomy surgical approaches are available to remove the uterus and resolve fibroid symptoms.
Learn more -
Myomectomy
Fibroids are removed while preserving the uterus, which is the best treatment option for women who want to have children in the future.
Learn more -
Uterine Artery Embolization
The relatively new treatment is an alternative to surgical removal of fibroids.
Learn more