Viral Hepatitis
Overview
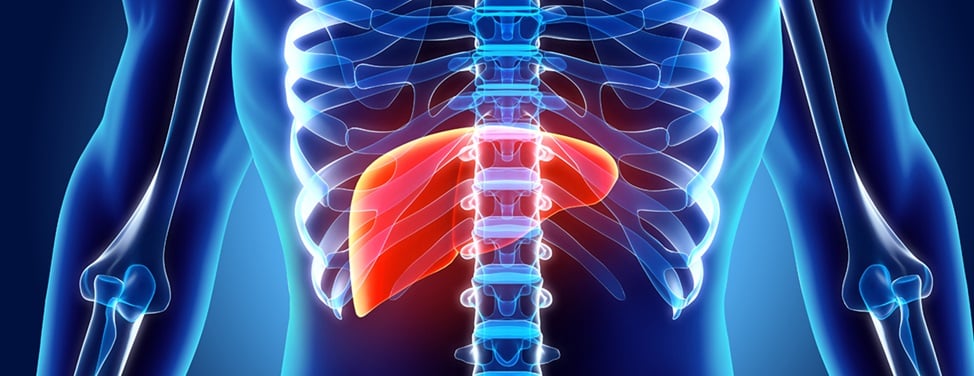
Viral hepatitis is an infection in the liver that causes liver inflammation and damage. There are several hepatitis viruses, including hepatitis A, B, C, D and E. The most common ones in the United States are hepatitis A, B and C.
Hepatitis A
Hepatitis A is spread through contaminated food or water. In most people, it causes an acute illness with fever, loss of appetite and jaundice lasting two to three weeks.
Most patients recover completely and then have lifelong immunity. But in some people, including those with pre-existing advanced liver disease, acute hepatitis A tends to be severe and can be fatal without a liver transplant.
Hepatitis B
Hepatitis B is primarily spread through exposure to the blood or other body fluids of someone living with hepatitis B, including through sexual contact. Newborns can acquire hepatitis B at birth if their mother has active hepatitis B, but medical treatments can prevent transmission.
Adults exposed to hepatitis B have an acute illness that ranges from very mild, with flu-like symptoms only, to more severe, with nausea, abdominal pain and jaundice. About 5 to 10% of adults exposed to hepatitis B develop a chronic infection. Most adults recover and are then immune to hepatitis B without risk of transmission to others. However, hepatitis B can return when people with a history of hepatitis B exposure are placed on medications that affect their immune system.
Most children who are exposed to hepatitis B develop a chronic infection. People with long-standing chronic hepatitis B spanning more than 20 years are at risk of developing cirrhosis and liver cancer.
Hepatitis C
Hepatitis C typically spreads through contact with blood. Currently, the most common way of being exposed is by sharing injection equipment, such as needles and syringes, with a person who has hepatitis C. (Before widespread blood bank screening began in 1992, blood transfusions were a common way of being exposed.)
The acute phase of hepatitis C illness is often very mild. Many people fail to clear the virus, however, and about 70% become chronically infected, with or without symptoms. An estimated 4 million Americans have hepatitis C — and many of them don't know it.
The virus causes inflammation that slowly and insidiously, over 20 to 30 years, leads to scarring of the liver. As the disease progresses, the first sign may simply be a lack of energy.
Later symptoms may include retention of fluid (causing swollen ankles), weight gain, internal bleeding and confusion. For reasons that are only partially understood, how quickly the disease progresses varies. But it's clear that heavy alcohol use accelerates it.
People who develop advanced scarring of the liver, a condition known as cirrhosis, have a significant risk of developing liver cancer.
Our approach to viral hepatitis
UCSF offers the most advanced diagnostic and treatment options for patients with all forms of viral hepatitis. Our approach depends on the type and severity of the disease.
Hepatitis A usually resolves on its own, so we help patients manage their symptoms and avoid spreading the infection. We treat chronic cases of hepatitis B or C with the latest medication therapies.
Chronic hepatitis infections can lead to severe liver damage or failure if patients don't respond to treatment or don't know they have the virus until symptoms of liver disease appear. In these cases, a liver transplant may be necessary.
Our Liver Transplant Program, designated a center of excellence by the Department of Health and Human Services, is known for outstanding outcomes and for helping pioneer techniques that have made transplants safer and more successful. We perform more than 200 transplants each year, and our survival statistics are among the very best in the country.
Awards & recognition
-

Among the top hospitals in the nation
-

Best in Northern California for gastroenterology & GI surgery
Signs & symptoms
As viral hepatitis becomes more advanced, it may cause one or more of the following symptoms:
- Loss of appetite
- Nausea and vomiting
- Fever
- Dark urine
- Stomach pain
- Fatigue
- Yellowing of the skin and eyes (jaundice)
- Mood change, forgetfulness
- Black bowel movements, a sign of intestinal bleeding
Diagnosis
To diagnose hepatitis, blood tests are used to detect the virus as well as antibodies to the virus. These tests also distinguish between acute and chronic infections.
Treatments
Treatment for hepatitis varies, depending on the type and severity of the disease.
Hepatitis A treatment
There's no specific therapy for acute hepatitis A infection, but resting, drinking plenty of liquids, and eating healthy food can help relieve symptoms.
If you think you've just been exposed, you may be able to prevent becoming infected by getting the hepatitis A vaccine or hepatitis A immunoglobulin. The vaccine is also recommended for anyone with liver disease and for people planning travel to areas of the world where sanitation may be less than optimal.
Before being vaccinated, you should get a blood test to check whether you already have antibodies to the virus. If you do, you won't need the vaccine.
Hepatitis B treatment
Hepatitis B usually isn't treated unless it becomes chronic and there's a risk of liver damage. In that case, your doctor may put you on one or more oral antiviral medications, such as entecavir (Baraclude), tenofovir alafenamide (Vemlidy) or tenofovir disoproxil fumarate (Viread).
These medicines interfere with the virus's ability to reproduce, and they slow its ability to damage the liver. They are taken for at least a year.
The disease can also be treated with injections of pegylated interferon, which boosts the immune system's ability to eliminate the virus. The shots are given weekly for six to 12 months.
An injection of immunoglobulin (an antibody) given within 24 hours of exposure to the virus may help protect you from getting sick with hepatitis B. Because this treatment provides only short-term protection, you should get the hepatitis B shot at the same time (if you've never had it).
The hepatitis B shot protects against the virus and is now part of the routine immunization schedule for babies. This vaccine is also recommended for children, adolescents and adults who haven't yet received it.
Hepatitis C treatment
In the past, hepatitis C was treated with a combination of injectable drugs that amped up the immune system to fight the virus. But they didn't reliably cure the disease, and often patients couldn't tolerate the side effects.
Now there's a better treatment: antiviral medications. These drugs fight the virus directly to keep it from multiplying.
There are many types of antiviral medicines. Each one works in a slightly different way, but they all come in pill form and are effective at curing the disease with minimal side effects.
The newest antivirals – known as direct-acting antivirals – have excellent outcomes, few side effects, and treatment times as short as eight weeks. Your doctor will choose the best medicine for you based on various factors, including your medical history, the type of hepatitis C you have and whether you have liver damage. The usual treatment course is eight to 12 weeks, but it can be longer.
Options include:
- Glecaprevir/pibrentasvir (Mavyret)
- Ledipasvir/sofosbuvir (Harvoni)
- Sofosbuvir/velpatasvir (Epclusa)
- Sofosbuvir, velpatasvir and voxilaprevir (Vosevi)
Your progress will be monitored throughout treatment. After treatment, you'll have blood tests regularly to check for the virus.
Liver transplants
A liver transplant may be an option for people whose hepatitis progresses to liver failure or liver cancer.
The evaluation for a transplant is complex and generally requires several months. To allow for that lengthy evaluation, even patients who feel well should be referred for a transplant at the first sign of liver failure. This is also true for patients who have advanced liver disease diagnosed by X-ray studies or a liver biopsy.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.
More treatment info
-
Living Donor Liver Transplant
The liver's unique ability to regenerate itself enables life-saving transplants.
Learn more -

Liver Transplant
Liver transplantation can be a life-saving option for patients with end-stage liver disease. Learn what happens during the evaluation, surgery and recovery.
Learn more