Heart Failure

Overview
What is heart failure?
Heart failure, also called congestive heart failure, doesn't mean that the heart has failed or stopped. It occurs when one or more chambers of the heart is failing to keep up with the normal volume of blood flow.
Heart failure can be the result of weakened heart muscles, stiffening of the heart chambers or problems with the valves. A heart attack or conditions like coronary artery disease, pulmonary hypertension or cardiomyopathies can contribute to heart failure.
People often live healthy lives by managing this condition with medication, lifestyle adjustments and other treatments.
Our approach to heart failure
UCSF is an internationally recognized leader in treating heart failure at all stages. Our program offers state-of-the-art conventional as well as experimental therapies, many of them developed right here.
Patients with advanced heart failure may benefit from mechanical circulatory support implants. Our doctors have experience with nearly every federally approved device, so they know how to find the right approach and device for each patient.
In heart failure's final stages, transplantation may be an option. UCSF's award-winning heart transplant program is one of the most active and effective in the region. Our team has performed hundreds of transplants in the last 25 years.
Awards & recognition
-

Among the top hospitals in the nation
-

One of the nation's best for heart & vascular care
-

Rated high-performing hospital for heart failure care
Causes of heart failure
Common causes of heart failure include the following:
- Heart attack. During a heart attack, also called a myocardial infarction, an artery that supplies blood to the heart is blocked, so no oxygen reaches the heart muscle. The resulting damage to the heart muscle can contribute to heart failure.
- Coronary artery disease (CAD). This condition occurs when the blood vessels become narrow, clogged or have blood clots lodged in them. When this happens, not enough blood reaches the heart, damaging the heart muscle and contributing to heart failure.
- Heart arrhythmia. This condition occurs when a person's heartbeat is too fast, too slow or irregular, making it difficult to pump enough blood. Once the underlying cause of the arrhythmia is treated, heart failure symptoms may go away.
- Cardiomyopathy or myocarditis. Heart muscle disease (cardiomyopathy) or inflammation (myocarditis) can damage the heart muscle, increasing the risk of heart failure.
- Diabetes. This condition tends to increase the levels of cholesterol and triglycerides – unhealthy fats that contribute to coronary artery disease. People with diabetes also are more likely to be overweight and have high blood pressure. These conditions can put extra strain on the heart, which can lead to heart failure, or other cardiovascular diseases.
- High blood pressure. Uncontrolled high blood pressure, or hypertension, doubles a person's risk of developing heart failure. If the pressure created by blood flow through the vessels is too high, the heart has to pump harder to keep the blood circulating. Over time, the extra burden can weaken the heart and eventually contribute to heart failure.
- Heart birth defects. If the heart and its chambers don't form correctly in the developing fetus, the healthy parts of the heart are forced to work harder. Over time, the added stress may cause healthy structures to fail.
- Abnormal heart valves. The valves that open and close to allow blood to pass between the chambers of the heart may be damaged by disease or infection or they may form improperly before birth. A faulty valve can cause the heart to pump harder to keep the blood moving. If the workload becomes too great, heart failure can develop.
- Alcohol and drug abuse. Excessive use of alcohol or substances such as cocaine or amphetamines can damage the heart. So can some prescription drugs. The impact they have on heart tissues or vessels can lead to heart failure or other heart diseases.
Less common causes of heart failure
Sometimes, a healthy heart can temporarily struggle to meet your body's oxygen and nutrient needs. This may be due to issues unrelated to the cardiovascular system. These problems are less common causes of heart failure, but they do pose some risk. Because of the potential risk, it's important to monitor your heart function if you have:
- Anemia. Red blood cells carry oxygen needed to maintain life in the body's cells. People with anemia do not have enough red blood cells. To compensate, the heart pumps at a faster rate, circulating the smaller number of red cells quickly enough to supply the body's oxygen needs. Over time, the extra burden may lead to heart damage.
- Hyperthyroidism. This condition is the result of an overactive thyroid, which causes the body to work at a faster pace. The increased pace can overwork the heart as it tries to keep up with the demand for oxygen and nutrients. This can lead to heart failure or other medical issues.
Other causes of heart failure
Factors related to lifestyle and family history can also contribute to heart failure, including:
- High cholesterol
- Smoking
- A family history of heart failure or other heart disease
Sometimes, there is no known cause for heart failure.
Types of heart failure
Heart failure may involve the left side, the right side or both sides of the heart. Each side of the heart has an upper chamber (an atrium) and a lower chamber (a ventricle). When any one of these chambers is not be able to keep up with the volume of blood flowing through it, the heart can malfunction.
Left-sided heart failure
The left side of the heart is crucial for normal heart function and is usually where heart failure begins. The left atrium receives oxygen-rich blood from the lungs and pumps it into the left ventricle, the heart's largest and strongest pump. This pump is responsible for supplying blood to the body.
The left side of the heart can malfunction in two different ways that lead to heart failure:
- Systolic heart failure. This is the most common type of heart failure. It occurs when the heart is weak and enlarged and the muscle of the left ventricle loses some of its ability to contract. When this happens, the muscle is unable to pump enough oxygen and nutrients into the blood to meet the body's needs.
- Diastolic failure. This type of heart failure occurs when the muscle in the left ventricle becomes stiff and loses some of its ability to relax. As a result, the affected chamber has trouble filling with blood during the rest period between each heartbeat. Often the walls of the heart thicken, and the size of the left chamber may shrink.
Right-sided heart failure
After the blood has circulated through the body, it returns to the right atrium and then travels to the right ventricle. The blood is then pumped it into the lungs to be replenished with oxygen. When the right side loses pumping power, the blood can back up in the veins while it is attempting to return to the heart.
Right heart failure may occur alone but is usually a result of left-sided failure. When the left ventricle fails, fluid backs up in the lungs. In turn, pressure from excess fluid can damage the heart's right side as it works to pump blood into the lungs.
Symptoms of heart failure
Heart failure is usually a chronic, or long-term, condition that gradually gets worse. By the time most people notice and see a doctor about their symptoms, the heart has been failing, little by little, for a long time.
This is a good reason to have regular health checkups. During a routine checkup, your doctor may detect signs of heart failure long before you experience symptoms. Heart failure rarely occurs suddenly except after a major heart attack, severe heart valve problem or period of seriously high blood pressure.
People who experience any symptoms of heart failure, even if they are mild, should consult a doctor as soon as possible. If you are diagnosed, it's important to keep track of these symptoms and report any sudden changes.
Common symptoms of heart failure
- Breathlessness or shortness of breath
- Fatigue
- Chronic cough or wheezing
- Rapid or irregular heartbeat
- Lack of appetite or nausea
- Mental confusion or impaired thinking
- Fluid buildup and swelling in the feet, ankles and legs
- Rapid weight gain
- Heart grows larger. The muscle mass of the heart grows to try and increase its pumping power, which works for a while. The heart chambers also enlarge and stretch so they can hold a larger volume of blood. As the heart expands, the cells controlling its contractions also grow.
- Heart pumps faster. To circulate more blood throughout the body, the heart speeds up.
- Blood vessels narrow. As less blood flows through the arteries and veins, blood pressure can drop to dangerously low levels. To compensate, the blood vessels become narrower, which keeps blood pressure higher, even as the heart loses power.
- Blood flow is diverted. When the blood supply is no longer able to meet all of the body's needs, it flows away from less-crucial areas, such as the arms and legs. The blood is diverted to the organs that are most important for survival, including the heart and brain. As a result, physical activity becomes more difficult as heart failure progresses.
- An enlarged heart eventually doesn't function as well as a normal heart, and the extra muscle mass adds stress to the entire cardiovascular system.
- The organ systems from which blood has been diverted may eventually deteriorate because they don't receive enough oxygen.
- Narrowing of the blood vessels limits the blood supply. This can contribute to conditions such as stroke, heart disease and clogged or blocked blood vessels in the legs and other parts of the body.
- Pumping blood too fast for too long can damage the heart muscle and interfere with its normal electrical signals, which can result in a dangerous heart rhythm disorder.
Typical signs of heart failure include:
Changes in heart function
Symptoms occur as the heart loses strength and its ability to pump blood throughout the body. As the heart functions fail, blood can back up and cause congestion in the lungs and other body tissues. This is why heart failure sometimes is called congestive. Excess fluid may also pool in the failing portion of the heart and the lungs.
Because it is too weak to pump properly, the heart and other parts of the body will attempt to adapt to the decline. When this happens, the:
Complications of heart failure
Although the body's ability to compensate for the failing heart is beneficial, in the long run these adaptations contribute to complications that can be very serious. For example:
Eventually, the heart and body are unable to keep up with the added stress. If you wait to see a doctor until you experience obvious symptoms of heart failure, the condition may already be life-threatening. If you experience any of these symptoms, consult your doctor as soon as possible.
Diagnosis of heart failure
To diagnose heart failure, your doctor will compile a complete medical history. They will also ask you about your symptoms and perform a physical exam.
They may do blood tests look at your kidney and liver function, sodium and potassium levels, blood count and other measurements.
Your doctor may also order the following tests:
- Chest X-ray. These images are used to check the size of your heart and see if there is excess fluid in the heart or lungs.
- Electrocardiogram (ECG or EKG). This is a simple, painless test that records the electrical activity of the heart through electrodes placed on the skin of the chest.
Ejection fraction and additional tests to diagnose heart failure
If X-rays or an ECG suggest heart failure, the next step will be an imaging study to evaluate the structure and function of the heart, and measure the heart's ejection fraction (EF). An EF evaluates the percentage of blood that the heart pumps out with each heartbeat. A normal heart pumps out one-half to two-thirds of the blood with each heartbeat. An EF below 40 percent indicates a weakened heart.
Based on your medical history and symptoms, the doctor will order one or more of the following tests to measure your EF and diagnose whether the problem is due to systolic or diastolic failure.
- Echocardiography. This is a safe, painless test that uses sound waves (ultrasound) to examine the heart's structure and motion. This test provides information about your heart's pumping ability, blood-flow activity, valve function, size and pressure.
- Radionuclide ventriculography. This test involves injecting a small amount of radioactive dye into your vein to create images that help measure your heart's pumping ability and electrical activity. This scan may be done twice – once when you are at rest and again when you are exercising.
- Exercise stress test. This test measures how much oxygen the heart can provide to your muscles while you exercise on a stationary bike or treadmill.
- Electrophysiology (EP) study. During this test, small flexible tubes called catheters are inserted through the blood vessels into the heart to record its electrical signals.
The doctor uses information from these tests to determine the type and severity of heart failure, the short-term outlook and the best course of treatment.
Classification of heart failure
After the diagnosis is confirmed, the doctor will usually classify, or rank, the level of heart failure based on the severity of your symptoms. The most commonly used classification system is called the New York Heart Association Functional Classification. Your heart failure is placed in one of four categories, depending on how your condition affects how you perform normal physical activities.
The four categories are:
- Class I. Patients in this category feel no symptoms and can perform ordinary physical activities without any limitations. They represent about 35 percent of patients with heart failure.
- Class II. Patients have mild symptoms, such as occasional swelling, and may be somewhat limited in their ability to exercise or do other strenuous activities. They don't feel symptoms when at rest. About 35 percent of patients with heart failure are in this class.
- Class III. Patients are limited in their ability to exercise or participate in mildly strenuous activities and are comfortable only at rest. About 25 percent of heart failure patients are in this class.
- Class IV. Patients are severely limited in their ability to perform any activity, having symptoms even while at rest. This is the most severe form of heart failure, occurring in about 5 percent of patients.
Treatment for heart failure
Although heart failure is a serious condition that gets progressively worse over time, certain cases can be reversed with treatment. Even when the heart muscle is damaged, there are several treatments that can relieve symptoms and stop or slow them.
The goals of heart therapy are to:
- Relieve symptoms and improve quality of life
- Slow disease progression
- Reduce the need for emergency room visits and hospitalization
- Help a person live longer
Treatment options depend on the type, cause, symptoms and severity of the heart failure. Usually, more than one therapy is used.
Treating the underlying causes of heart failure
A number of conditions can contribute to heart failure. Depending on the condition, treatment can range from surgery or angioplasty to medications. It's also important to treat arrhythmias in patients with heart failure.
Lifestyle changes for heart failure
Heart failure recovery and even prevention can start with simple lifestyle changes. These changes often improve or control some of the factors that contribute to heart failure.
Many people with heart failure will see an improvement if they:
- Modify daily activities and get enough rest to avoid stressing the heart
- Eat a heart-healthy diet that is low in sodium and fat
- Don't smoke and avoid exposure to secondhand smoke
- Don't drink alcohol or limit intake to no more than one drink two or three times a week
- Lose weight
- Avoid or limit caffeine intake
- Get regular exercise, which may include a physical rehabilitation program, once symptoms are stable
- Reduce stress
- Weigh themselves daily (a sudden increase may signal fluid build-up)
- Keep track of symptoms and report any changes
- Have regular checkups to monitor the condition
Medications for heart failure
A number of medications are used to treat heart failure, and most patients will need to take a combination of them. Medications may be prescribed to dilate blood vessels, strengthen the heart's pumping action or to reduce water and sodium in the body to lessen the heart's workload.
Medications for heart failure may include:
- Angiotensive converting enzyme (ACE) inhibitors. These dilate, or widen, the arteries, improving blood flow so that the heart doesn't have to pump as hard.
- Beta-blockers. These lower blood pressure and decrease and block the effect of harmful hormones that can cause disease progression.
- Diuretics or water pills. These help the kidneys produce more urine and rid the body of excess fluid, which can stress the heart.
- Spironolactone. This is a diuretic that preserves potassium and has been shown to reduce hospitalization and prolong life when used to treat advanced heart failure.
- Potassium and magnesium supplements. These are often prescribed with diuretics to replace these minerals, which are excreted in urine.
- Digoxin. This makes the heart beat stronger and slower and regulates the rhythm of its contractions.
- Anti-arrhythmic drugs. These drugs treat abnormal heart rhythms.
Surgery for conditions related to heart failure
In cases where another condition is the underlying cause of heart failure, that condition may require surgery. If the surgery is effective, if should also relieve the symptoms associated with heart failure.
Coronary artery bypass graft (CABG or cabbage)
This procedure can help prevent and treat heart failure caused by blocked arteries. The surgeon takes blood vessels from another part of the body – usually the leg – and then attaches them to the clogged artery to create a detour around the blockage. This is typically done through open-heart surgery, but some patients may be candidates for minimally invasive CABG, an alternative offered at UCSF Health.
Angioplasty
Angioplasty is another treatment for blocked arteries. This procedure involves inserting a thin flexible tube, called a catheter, through a small incision in the groin or neck and threading it through blood vessels until it reaches the one that is blocked.
In a balloon angioplasty, a balloon is inserted through the catheter into the center of the blocked artery. Once there, the balloon is inflated to compress the blockage material against the walls of the artery. With an angioplasty with stent, a small metal device, called a stent, may also be inserted through the catheter as a permanent solution to keep the plaque compressed. In another type of angioplasty procedure, instruments are introduced through the catheter to remove the plaque.
Implants
Devices such as pacemakers and artificial heart valves can be used to correct underlying conditions like arrhythmias and heart valve disorders.
Repairing heart birth defects
The surgery to repair a birth, or congenital, heart defect depends on the specific type of defect and how serious it is. Simple heart defects usually improve on their own over time and may not need any treatment. But for more complex congenital heart defects that can lead to heart failure, surgery may be required.
Surgery for heart failure
Some surgeries are specifically designed to treat heart failure.
Heart transplantation
A heart transplant may be the best option for patients with the most severe types of heart failure. However, this treatment is only available to a small number of people due to a shortage of donor hearts. There have also been significant advances in artificial heart transplantation, so this may an option in the future.
Ventricular assist devices (VAD)
A ventricular assist device, also known as a VAD, is a mechanical pump designed to support heart function and maintain blood flow in a weak or failing heart. The device is surgically placed inside the body. It works by pumping blood from the lower chambers of the heart to the rest of the body. A VAD may be used long-term or as a temporary treatment for someone waiting for a heart transplant.
Heart reconstruction
The electrical signals that cause the heart to contract, move in a spiral pattern. Ideally the heart is an elliptical shape, like a football. This shape makes it easier to receive the electrical signals that trigger heartbeats. In heart failure, the heart often gets larger and become spherical, more like a basketball. This new shape means that the heart no longer "fits" the electrical pattern, making the system less efficient. A variety of surgical procedures can be used to reconstruct the heart to restore its proper shape. You and your doctor can discuss if any of these options is right for you.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.
Explore what we do
UCSF's 35 years of heart transplant experience
A leader in treating advanced heart failure, UCSF performed nearly 80 heart transplants in 2023. Learn about our team's commitment to cutting-edge technologies and techniques.
More treatment info
-

Implantable Cardioverter Defibrillator (ICD)
Learn how implantable cardioverter defibrillators (ICDs) use special pacing to help manage fast heartbeats and irregular heart rhythms.
Learn more -
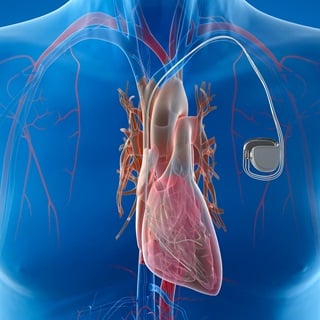
Pacemaker
Millions of people now rely on these tiny electronic devices to keep their hearts beating steadily.
Learn more -
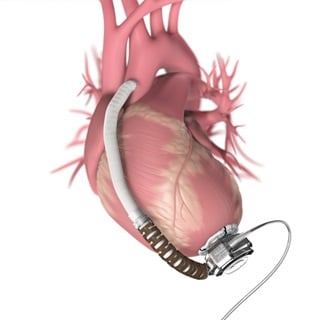
Ventricular assist device (VAD)
A mechanical pump is implanted in the chest to support heart function and improve blood flow in patients with weak or failing hearts.
Learn more