Metabolic Dysfunction–Associated Steatotic Liver Disease

Overview
Metabolic dysfunction–associated steatotic liver disease (MASLD), previously called nonalcoholic fatty liver disease (NAFLD), is a condition marked by excess fat in the liver. (MASLD is still commonly referred to as fatty liver disease.) Metabolic dysfunction–associated steatohepatitis (MASH) is an aggressive form of the condition in which the liver becomes inflamed. This can cause complications, including cirrhosis (tissue changes and damage to the liver).
In most people, MASLD occurs in tandem with other conditions, such as obesity, diabetes, high blood pressure or high cholesterol. Genetic factors, including a family history of diabetes or high cholesterol, may also play a role.
MASLD typically shows up as an unexpected abnormality in liver function tests – usually the alanine aminotransferase (ALT) and aspartate transaminase (AST) blood tests – in people who feel well. The elevation of the test result is usually minor and doesn't indicate a serious liver condition in younger patients. However, if the underlying cause of MASLD (such as obesity, diabetes, high blood pressure or high cholesterol) isn't treated, the condition may progress.
In people older than 50, MASLD may be diagnosed along with cirrhosis, the formation of scar tissue that can seriously damage the liver. About 20% of MASLD cases progress to cirrhosis. Studies are underway to further explore the link between the two conditions.
As the prevalence of obesity has increased in the United States, the incidence of MASLD has also risen. As a result, the condition is now among the most common reasons for liver transplantation.
Our approach to MASLD
Treatment for MASLD focuses on addressing its underlying cause, which is often obesity, diabetes or both. Successful treatment can halt or at least slow damage to the liver.
If the liver becomes too damaged to function, liver transplantation may be an option. UCSF's liver transplant program is renowned for outstanding outcomes, with survival rates among the best in the country. Our physician-scientists helped pioneer techniques that have improved the safety and effectiveness of transplantation for patients at UCSF and beyond.
Awards & recognition
-

Among the top hospitals in the nation
-

Best in Northern California for gastroenterology & GI surgery
Signs & symptoms
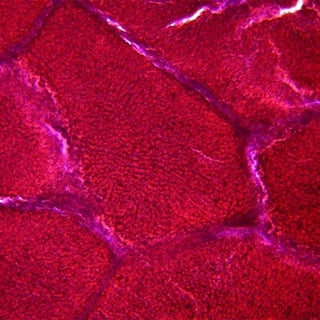
MASLD typically progresses over a period of years, even decades, with each stage of fibrosis (scarring) lasting an average of seven years. The disease goes through the following stages:
- Stage 0-1 (healthy liver). No significant liver damage has occurred.
- Stage 2 (fatty liver). Fat deposits lead to liver enlargement.
- Stage 3 (liver fibrosis). Scar tissue forms.
- Stage 4 (cirrhosis). New connective tissue grows, destroying healthy liver cells.
Signs and symptoms of MASLD vary widely, depending on the stage. During early and middle stages, patients often have no symptoms of liver disease.
However, as the disease advances, liver scarring may cause symptoms that include:
- Fatigue
- Memory loss or confusion
- Fluid retention in the abdomen or legs
- Passage of tarry black stools, indicating internal bleeding
Diagnosis
MASLD is often found incidentally, as part of testing for an unrelated problem. To confirm the diagnosis, your provider may order the following tests:
- Blood tests. Certain tests can measure liver function and detect inflammatory activity; other blood tests may be used to rule out viral hepatitis (liver inflammation caused by certain viruses).
- Liver ultrasound. This simple imaging procedure can show irregularities in the liver's shape and consistency as well as problems involving the biliary tract, such as gallstones.
- Computed tomography (CT). In this imaging method, an X-ray beam rotates around the patient and a computer creates a detailed view of structures within the body, such as the liver.
- Liver biopsy. In some cases, providers need this to make a definitive diagnosis. The biopsy results also help define the stage of MASLD and severity of liver inflammation. To obtain a small tissue sample for analysis, a needle is inserted into the liver. The procedure is performed in the clinic under local anesthesia (medications that prevent pain in a specific area).
Treatments
For patients with obesity and high levels of damaging bloodstream lipids (fat), weight loss is the recommended treatment for MASLD. If patients are able to lose weight and maintain the weight loss, MASLD and MASH can be reversed.
For patients with diabetes, high blood pressure or high cholesterol, controlling blood sugar levels can help prevent additional liver injury. All patients with MASLD should avoid alcohol, highly processed foods and foods with high levels of added sugar.
Therapeutic options for MASLD are evolving rapidly. UCSF is involved in numerous clinical trials and other studies investigating promising new medications for MASLD, as well as other innovative treatment approaches.
Liver transplantation
In some cases, MASLD may progress to liver failure and require liver transplantation. The evaluation for a transplant is complex and generally requires several months. Therefore, even patients who feel well should be referred for a transplant at the first sign of liver failure or if they have advanced liver disease diagnosed by X-ray studies or liver biopsy.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.
More treatment info
-
Living Donor Liver Transplant
The liver's unique ability to regenerate itself enables life-saving transplants.
Learn more -

Liver Transplant
Liver transplantation can be a life-saving option for patients with end-stage liver disease. Learn what happens during the evaluation, surgery and recovery.
Learn more