Brain Tumor
Overview
Early diagnosis can be an important factor in the outcome of tumors in the brain. Brain tumors are the second leading cause of cancer death in children under age 15 and the second fastest growing cause of cancer death among those over age 65. Over the next year, more than 100,000 people in the United States will be diagnosed with a brain tumor.
Types of brain tumors
Primary brain tumors
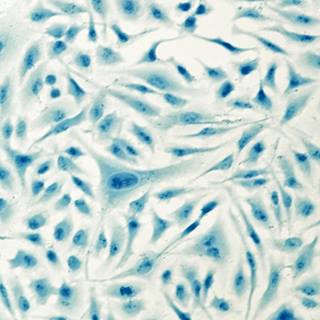
Tumors that begin in brain tissue are known as primary brain tumors and are classified by the type of tissue in which they originate. The most common brain tumors are gliomas, which begin in the glial or supportive tissue. There are several types of gliomas:
- Astrocytomas. These tumors arise from small, star-shaped cells called astrocytes. They may grow anywhere in the brain or spinal cord. In adults, astrocytomas most often arise in the cerebrum. In children, they occur in the brain stem, the cerebrum and the cerebellum. A grade III astrocytoma is sometimes called anaplastic astrocytoma. A grade IV astrocytoma is usually called glioblastoma multiforme.
- Brain stem gliomas. These tumors occur in the lowest, stem-like part of the brain. The brain stem controls many vital functions. Most brain stem gliomas are high-grade astrocytomas.
- Ependymomas. These tumors usually develop in the lining of the ventricles. They may also occur in the spinal cord. Although these tumors can develop at any age, they are most common in childhood and adolescence.
- Oligodendrogliomas. These tumors occur in the cells that produce myelin, the fatty covering that protects nerves. These tumors usually arise in the cerebrum. They are rare, grow slowly and usually do not spread into surrounding brain tissue. They occur most often in middle-aged adults but have been found in people of all ages.
There are other types of brain tumors that do not begin in glial tissue. Some of the most common are described below:
- Medulloblastomas. These tumors were once thought to develop from glial cells. However, recent research suggests that these tumors develop from primitive or developing nerve cells that normally do not remain in the body after birth. For this reason, medulloblastomas are sometimes called primitive neuroectodermal tumors (PNET).
Most medulloblastomas arise in the cerebellum; however, they may occur in other areas as well. These tumors occur most often in children and are more common in boys than in girls. - Meningiomas. These tumors grow from the meninges, or membranes that enclose the brain and spinal cord. They are usually benign. Because these tumors grow very slowly, the brain may be able to adjust to their presence. Meningiomas often grow quite large before they cause symptoms. They occur most often in women between 30 and 50 years of age.
- Schwannomas. These tumors are benign and begin in Schwann cells, which produce the myelin that protects the acoustic nerve, or the nerve of hearing. They occur mainly in adults. These tumors affect women twice as often as men.
- Craniopharyngiomas. These tumors develop in the region of the pituitary gland near the hypothalamus. They are usually benign but are sometimes considered malignant because they can press on or damage the hypothalamus, a region of the brain, and affect vital functions. These tumors occur most often in children and adolescents.
- Germ cell tumors. These tumors arise from developing sex cells or germ cells. The most frequent type of germ cell tumor in the brain is the germinoma.
- Pineal region tumors. These tumors occur in or around the pineal gland, a tiny organ near the center of the brain. The tumor can be slow growing (pineocytoma), or fast growing (pineoblastoma). The pineal region is very difficult to reach, and these tumors often cannot be removed.
Secondary brain tumors
Metastasis is the spread of cancer. Cancer that begins in other parts of the body may spread to the brain and cause secondary tumors. These tumors are not the same as primary brain tumors. Cancer that spreads to the brain is the same disease and has the same name as the original or primary cancer. For example, if lung cancer spreads to the brain, the disease is called metastatic lung cancer because the cells in the secondary tumor resemble abnormal lung cells, not abnormal brain cells.
Treatment for secondary brain tumors depends on where the cancer started and the extent of the spread as well as other factors, including the patient's age, general health and response to previous treatment.
Our approach to brain tumor
As one of the largest and most comprehensive brain tumor programs in the U.S., we are committed to providing the best possible outcomes and quality of life to our patients. We offer the latest treatments and techniques, such as brain mapping during surgery to protect brain function and radiosurgery, a nonsurgical treatment that delivers high radiation doses to a precise target in the brain. Our patients also have access to clinical trials evaluating promising new treatments, and to supportive care and resources for themselves and their families.
Explore what we do
Brain tumor tests lead to better outcomes
Using new tools for more precise diagnoses and treatments, the UCSF Brain Tumor Center helps patients like Kelly live longer.
Awards & recognition
-

Among the top hospitals in the nation
-

Best in California and No. 2 in the nation for neurology & neurosurgery
-

Best in Northern California and No. 7 in the nation for cancer care
-

in the U.S. for number of brain tumor patients treated
Signs & symptoms
The symptoms of brain tumors depend on their size and location in the brain. Symptoms often are caused by damage to vital tissue and pressure on the brain as the tumor grows within the limited space in the skull. They may be caused by swelling and a buildup of fluid around the tumor, a condition called edema. Symptoms also may be due to hydrocephalus, which occurs when the tumor blocks the flow of cerebrospinal fluid and causes a build-up in the ventricles.
If a brain tumor grows very slowly, its symptoms may not appear for some time. The most frequent symptoms of brain tumors include:
- Headaches that tend to be worse in the morning and ease during the day
- Seizures or convulsions
- Nausea or vomiting
- Weakness or loss of feeling in the arms or legs
- Stumbling or lack of coordination in walking
- Abnormal eye movements or changes in vision
- Drowsiness
- Changes in personality or memory
- Changes in speech
These symptoms may be caused by brain tumors or by other problems. Diagnostic tests can be performed to determine if the cause of your symptoms is a brain tumor and if it is a primary or secondary one.
Diagnosis
To find the cause of your symptoms, your doctor will ask about your personal and family medical history and perform a complete physical examination. In addition to checking general signs of health, your doctor will perform a neurologic exam. This includes checks for alertness, muscle strength, coordination, reflexes and response to pain. Your doctor also examines the eyes to look for swelling caused by a tumor pressing on the nerve that connects the eye and the brain.
Depending on the results of the physical and neurologic examinations, your doctor may request one or both of the following:
- Computerized tomography (CT) Scan. Computerized tomography (CT) or computerized axial tomography (CAT) scan is a series of detailed pictures of the brain, created by a computer linked to an X-ray machine. In some cases, a special dye is injected into a vein before the scan. The dye helps to show differences in the tissues of the brain.
- Magnetic resonance imaging (MRI). Magnetic resonance imaging (MRI) provides pictures of the brain, using a powerful magnet linked to a computer. MRI is especially useful in diagnosing brain tumors because it can "see" through the bones of the skull to the tissue underneath. A special dye may be used to enhance the likelihood of detecting a brain tumor.
The doctor may also request other tests such as:
- Angiogram or arteriogram. These tests are a series of X-rays taken after a special dye is injected into an artery, usually in the area where the abdomen joins the top of the leg. The dye, which flows through the blood vessels of the brain, can be seen on X-rays. These X-rays can show the tumor and connecting blood vessels.
- Brain scan. A brain scan reveals areas of abnormal growth in the brain and records them on special film. A small amount of a radioactive material is injected into a vein. This dye is absorbed by the tumor and the growth shows up on the film. The radiation leaves the body within six hours and is not dangerous.
- Functional imaging. This test utilizes MRI or magnetic source imaging to identify functional pathways in the brain (motor, visual, language) and alerts the surgeon to potential injury to these pathways during surgery before damage could occur.
- Myelogram. A myelogram, sometimes called a lumbosacral spine X-ray, is an X-ray or computerized tomography (CT) scan of the spine. A special dye is injected into the cerebrospinal fluid in the spine and the patient is tilted to allow the dye to mix with the fluid. This test may be done when the doctor suspects a tumor in the spinal cord.
- MR spectroscopy. This is a modified MRI scan that shows metabolic activity within a brain tumor. This has largely replaced positron emission tomography (PET) scanning due to its superior resolution and accuracy.
Treatments
Treatment for brain tumors depends on a number of factors including the type, location and size of the tumor as well as the patient's age and general health. Treatment methods and schedules differ for children and adults.
Brain tumors are treated with surgery, radiation therapy and chemotherapy. Our doctors also are studying a vaccine for treating a recurrent cancer of the central nervous system that occurs primarily in the brain, known as glioma.
Depending on your needs, several methods may be used. Our team includes neurosurgeons, medical oncologists, radiation oncologists, nurses, a dietitian and a social worker, who work together to provide the best possible care.
Before treatment begins, most patients are given steroids, drugs that relieve swelling or edema. Your may receive anticonvulsant medicine to prevent or control seizures.
If hydrocephalus is present, you may need a shunt to drain cerebrospinal fluid. A shunt is a long, thin tube placed in a ventricle of the brain and then threaded under the skin to another part of the body, usually the abdomen. It works like a drainpipe. Excess fluid is carried away from the brain and is absorbed in the abdomen. In some cases, the fluid is drained into the heart.
Surgery
Surgery is the usual treatment for most brain tumors. To remove a brain tumor, a neurosurgeon makes an opening in the skull. This operation is called a craniotomy. Whenever possible, the surgeon attempts to remove the entire tumor. If the tumor cannot be completely removed without damaging vital brain tissue, your doctor may remove as much of the tumor as possible. Partial removal helps to relieve symptoms by reducing pressure on the brain and reduces the amount of tumor to be treated by radiation therapy or chemotherapy.
Some tumors cannot be removed. In such cases, your doctor may do only a biopsy. A small piece of the tumor is removed so that a pathologist can examine it under a microscope to determine the type of cells it contains. This helps your doctor decide which treatment to use.
Sometimes, a biopsy is done with a needle. Doctors use a special head frame (like a halo) and CT scans or MRI to pinpoint the exact location of the tumor. The surgeon makes a small hole in the skull and then guides a needle to the tumor. Using this technique to do a biopsy or for treatment is called stereotaxis.
Other advanced techniques during surgery include brain mapping to find functional pathways near tumors, endoscopy to perform biopsies and open spinal fluid pathways through a small scope and advanced frameless stereotaxic computer assisted tumor resections. Intraoperative MRI also is available to help maximize tumor removal.
Radiation therapy
Radiation therapy, also called radiotherapy, is the use of high-powered rays to damage cancer cells and stop them from growing. It is often used to destroy tumor tissue that cannot be removed with surgery or to kill cancer cells that may remain after surgery. Radiation therapy also is used when surgery is not possible.
Radiation therapy may be given in two ways. External radiation comes from a large machine. Generally, external radiation treatments are given five days a week for several weeks. The treatment schedule depends on the type and size of the tumor and your age. Giving the total dose of radiation over an extended period helps to protect healthy tissue in the area of the tumor.
External radiation may be directed just to the tumor, the surrounding tissue or the entire brain. Sometimes the radiation is also directed to the spinal cord. When the whole brain is treated, the patient often receives an extra dose of radiation to the area of the tumor. This boost can come from external radiation or from an implant.
Radiation also can come from radioactive material placed directly in the tumor, or implant radiation therapy. Depending on the material used, the implant may be left in the brain for a short time or permanently. Implants lose a little radioactivity each day. The patient stays in the hospital for several days while the radiation is most active.
The Gamma Knife, or stereotactic radiosurgery, is another way to treat brain tumors. The Gamma Knife isn't actually a knife, but a radiation therapy technique that delivers a single, finely focused, high dose of radiation precisely to its target. Treatment is given in just one session. High-energy rays are aimed at the tumor from many angles. In this way, a high dose of radiation reaches the tumor without damaging other brain tissue.
Chemotherapy
Chemotherapy is the use of drugs to kill cancer cells. The doctor may use just one drug or a combination, usually giving the drugs orally or by injection into a blood vessel or muscle. Intrathecal chemotherapy involves injecting the drugs into the cerebrospinal fluid.
Chemotherapy is usually given in cycles. A treatment period is followed by a recovery period, then another treatment period and so on. Patients often don't need to stay in the hospital for treatment and most drugs can be given in the doctor's office or clinic. However, depending on the drugs used, the way they are given and the patient's general health, a short hospital stay may be necessary.
Advances in chemotherapy include direct placement into the tumor cavity using a new technique called convection enhanced delivery.
UCSF Health medical specialists have reviewed this information. It is for educational purposes only and is not intended to replace the advice of your doctor or other health care provider. We encourage you to discuss any questions or concerns you may have with your provider.
More treatment info
-

Brain Mapping
This is the most common surgical treatment for epilepsy. It involves removing a small area of brain tissue where the seizures originate.
Learn more -
Brachytherapy (HDR & LDR)
Radioactive material is placed inside a tumor or very close to it to treat the tumor and spare healthy tissue.
Learn more -
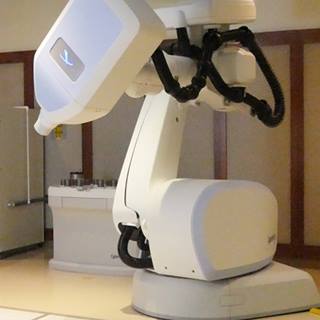
CyberKnife
Radiosurgery minimizes radiation exposure to healthy tissue surrounding a tumor and offers rapid relief from pain and other symptoms.
Learn more -

Gamma Knife
An advanced radiation procedure used to treat neurological conditions including tumors, epilepsy, trigeminal neuralgia and arteriovenous malformations.
Learn more
Recommended reading
Where to get care (2)
Patient stories
Related clinics (4)

Osher Center for Integrative Health
 2
2